What works: Improving case finding of long-term health problems in disadvantaged communities

Millions of people in England have an undiagnosed health problem, with people living in socioeconomically disadvantaged areas more likely to be unaware of a health problem. In this evidence brief we explore what works to improve case finding for disadvantaged groups, specifically those lower socioeconomic and ethnic minority groups.
What works – improving case finding of long-term health problems in disadvantaged communities[PDF 267kb]
Download documentSummary
Millions of people in England have an undiagnosed health problem, with people living in socioeconomically disadvantaged areas more likely to be unaware of a health problem. Case finding is an approach to identifying people with undiagnosed health problems. There are already national programs, such as NHS Health Checks and hypertension case finding in pharmacies.
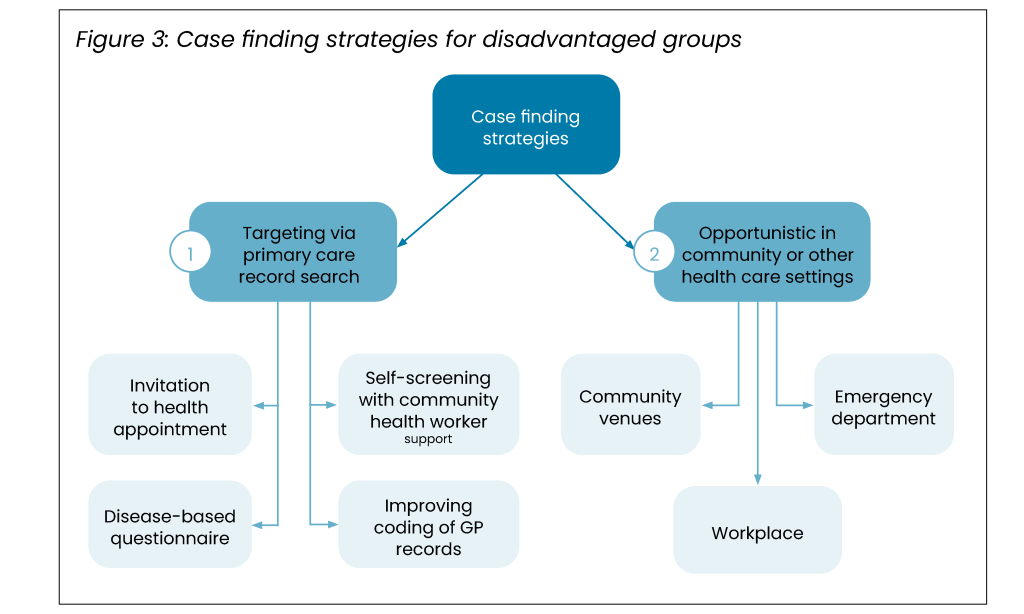
Here we explore what works to improve case finding for disadvantaged groups, specifically those lower socioeconomic and ethnic minority groups. Based on an evidence review, we found two main approaches to case finding: 1) searching the electronic health record in primary care and targeting patients or 2) opportunistically screening patients in the community, workplace or when they attend the emergency department. There is unlikely to be a single intervention which identifies the majority of patients, but rather a multicomponent intervention is likely to be most effective. Any case finding programme needs adequate diagnostic and management resources.
We found evidence to support:
- targeted searches in primary care electronic health records
- improving diagnostic codes in primary care
- case finding for chronic obstructive pulmonary disease (COPD) with disease-specific questionnaires
- cervical cancer self-screening for people who do not attend the national screening programme
- health checks in community venues, such as mosques and bus stations, workplace hypertension and cardiovascular disease screening and follow-up of people who are found to have high blood pressure in the emergency department.
Definitions
Case finding is a strategy for targeting resources at individuals or groups who are suspected to be at risk for a particular disease. It involves actively searching systematically for at-risk people, rather than waiting for them to present with symptoms or signs of active disease.
Screening is a strategy to detect early disease or risk factors for disease in large numbers of apparently healthy individuals [5].
Current challenges
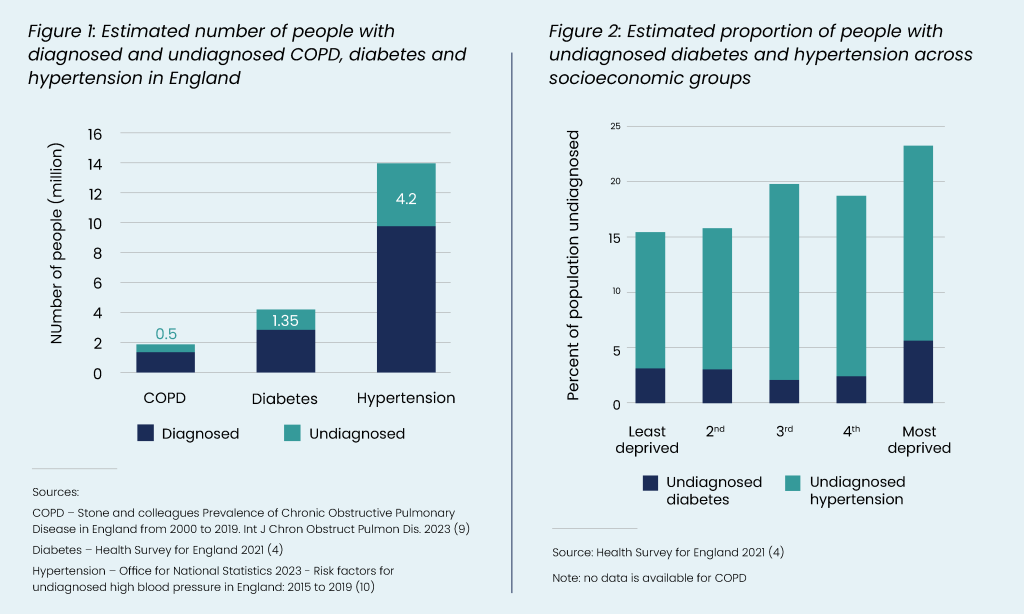
The greatest burden of illness from many long-term conditions is among the poorest in society. The most socioeconomically disadvantaged communities have at least a 50% higher prevalence of cardiovascular disease (CVD), diabetes, chronic pain, substance misuse and anxiety and depression [1]. Chronic obstructive pulmonary disease (COPD), a smoking related lung disease, is three times more common in the most deprived populations [1]. Some ethnic minority groups also have higher CVD, COPD and diabetes prevalence and complications. For example, South Asian minority groups are at increased risk of CVD and have mortality rates almost 50% higher when compared to non-South Asian populations [1][[2][3]. Furthermore, people living in poorer areas are more likely to have an undiagnosed health problem. The Health Survey for England found that there are twice as many people with undiagnosed diabetes in deprived areas compared to affluent areas and 50% more people with undiagnosed hypertension [4].
Costs to the NHS of long-term conditions are significant. CVD alone costs the NHS £9 billion annually, with annual costs to the UK economy estimated to be £19 billion [6]. COPD is estimated to cost more than £1.5 billion to the NHS each year [7]. Previous research has estimated that 40% of people with COPD are of working age, and a quarter of those are unable to work [8].
Many of these conditions have no or only mild symptoms, going undetected for long periods and missing opportunities for prevention or early treatment. There are an estimated 4.2 million people with undiagnosed hypertension, 1.35 million with undiagnosed diabetes and 500,000 with undiagnosed COPD [4][9][10]. Based on data from the Health Survey for England and a study of primary care records, the number with undiagnosed high cholesterol is even higher at 9.9 million [11].
It is estimated that £68bn could be saved, 4.9 million quality adjusted life years (QALYs) gained, and 3.4 million CVD cases prevented over 25 years if those in England with the six CVD high risk conditions (hypertension, diabetes, non-diabetic hyperglycaemia, atrial fibrillation, chronic kidney disease and high cholesterol) were diagnosed and managed at current levels [12].
Considering the significant impact of underdiagnosis, multiple NHS programmes have been initiated to identify undiagnosed health problems. The NHS health check programme aims to reduce morbidity and mortality from CVD, type 2 diabetes and chronic kidney disease through identification, treatment and education. Tanner and colleagues reviewed 29 studies on the NHS health checks and found that the programme led to increased diagnosis of risk factors and health problems including diabetes mellitus, hypertension, raised blood pressure, cholesterol and chronic kidney disease [13]. However, men, younger people and those from the most deprived areas were least likely to attend. In 2021 NHS England launched a pharmacy-based hypertension case finding service. Between April 2023 and March 2024, there were 1.7 million hypertension checks undertaken [14]. No data is available as to the outcomes of these checks.
Given the significant individual and collective costs of undiagnosed long-term conditions, especially in disadvantaged groups, finding a solution is vital. Better identification and management of these risk factors and conditions would improve health and reduce costs. Here we review the evidence of what works to identify people from disadvantaged background, specifically lower socioeconomic and ethnic minority groups, with undiagnosed health conditions through case finding. Population screening programmes are beyond the scope of this brief, but we do include key evidence for case finding in women who do not respond to the national cervical cancer screening programme.
Summary of evidence
We screened 667 review articles (93 from the Health Equity Evidence Centre Living Evidence Maps of what works to address inequalities and 570 from MEDLINE). Subsequent snowball searching using an AI tool (Litmaps) identified further relevant articles. We prioritised latest reviews and those of greatest relevance to the UK context. Our focus was on interventions which facilitate the identification of undiagnosed long-term conditions in disadvantaged groups. In total we included 22 studies. Some of the included studies did not directly focus on disadvantaged groups, however they have been included as they provide transferable evidence.
We found two main starting points for case finding of disadvantaged groups: 1) searching the primary care electronic patient record to identify at-risk people and engaging with them and 2) opportunistic engagement in the community, workplace or when patients attend other health care settings, such as the emergency department.
Our evidence review found multiple strategies that support the identification of health problems in disadvantaged groups. It is unlikely that a single programme or intervention will identify the majority of cases, but rather a multicomponent programme that seeks to identify cases through multiple approaches and settings.
1. Interventions initiated through primary care electronic health record (EHR)
In primary care, targeting patients through searches of the electronic patient record is more effective than opportunistic case finding, such as receptionists or GPs opportunistically asking people when they attend the surgery. Hemming and colleagues (2016) undertook a randomised controlled trial exploring whether targeted case-finding for prevention of CVD is more effective than opportunistic case-finding in primary care [15]. A nurse in primary care identified high risk (CVD risk of >20%) and undiagnosed patients between 35-74 years from patient records. Patients were invited for assessment (including BP measurement) and referred appropriately to their GP for treatment if required. The study showed that 19.7% of patients in the targeted group versus 10.8% of patients in the opportunistic case finding group were diagnosed and prescribed antihypertensives or statins.
A recent pilot study in Derby aimed to increase hypertension case finding in disadvantaged groups [16]. General practice staff searched the electronic health records to identify patients over 40 years old who were at higher risk of cardiovascular disease, less likely to attend healthcare and who had not had a BP reading for at least five years. Patients were invited for a BP check at the GP, mobile units or at other community locations with support from outreach health workers and interpreters. The general practice staff undertook 3,224 BP checks and a third were found to have hypertension.
Kypridemos and colleagues undertook a microsimulation study to compare the current model of universal health checks (i.e. everyone 40-74 years without pre-existing health problems) compared to targeting the most deprived areas [17]. The authors found the universal screening would avoid 19,000 CVD events and 3000 deaths. Whereas the targeted approach to the most disadvantaged 40% of the population would avoid 17,000 events and 2,000 deaths for considerably fewer resources.
These three studies taken together demonstrate that targeting is more effective than opportunistic screening in general practice and can be especially effective in disadvantaged groups. Furthermore, while universal health checks may avoid more events, the greatest returns on investment are when they are targeted at the disadvantaged communities.
EHR search followed by disease-based questionnaire
COPD has a high prevalence in socioeconomically disadvantaged areas. One Dutch study compared case finding for COPD in practices in low, moderate and high socioeconomic areas using patient questionnaires. They found more high-risk individuals (older and more current smokers) and more cases of COPD in the low SES practices compared to in moderate or high SES practices [18].
Patient questionnaires and handheld flow meters may be combined with searches of the electronic health record to identify people at risk of COPD. It is particularly suited to COPD because there are currently substantial waiting times for spirometry, the medical investigation required for a diagnosis, and since 90% of people with COPD have previously smoked they can be identified by smoking records [19].
The CAPTURE symptom questionnaire with or without peak flow measurement, a handheld device for helping diagnosis lung problems, is one example that has been shown to be sensitive and specific in identifying COPD that requires treatment [20]. The TargetCOPD score uses a risk score incorporating smoking status, respiratory symptoms and other risk factors using routine primary care data to identify high risk patients [21].
The TargetCOPD trial was a major UK-based cluster-randomised control trial with over 74,000 participants comparing targeted case finding for COPD to usual care [22]. Participants were randomised to receive screening questionnaires opportunistically during visits to the GP or actively where questionnaires and reminders were posted to eligible participants in addition to opportunistic screening. Those who scored highly for respiratory symptoms were offered referral for diagnostic spirometry. Targeted case finding identified statistically significantly more undiagnosed COPD compared to opportunistic case finding (4% vs 1%). A subsequent analysis found that patients diagnosed through COPD case finding were less likely to be added to the COPD register and less likely to offered support for their condition [23]. Long term data from TargetCOPD found no difference in hospitalisations or mortality between the groups over 4 years [24].
A cost-effectiveness analysis of TargetCOPD found that it was more cost effective than opportunistic case finding [25]. Active case finding for COPD compared to opportunistic case finding had an incremental cost effectiveness ratio (ICER) of £16,596 per quality adjusted life year (QALY). A Canadian budget impact analysis modelled the total medical costs of eight different opportunistic COPD case finding strategies [26]. The researchers found a symptom questionnaire and diagnostic spirometry was most cost-effective with a total budget cost of $423 million. A similar microsimulation economic analysis in China evaluated cost-effectiveness of a population wide case finding programme [27]. They found that case finding with a symptom questionnaire and handheld flow meters offered to the entire population over 35 years old (irrespective of smoking status) was the most cost-effective.
Identification of non-responders of cervical screening followed by self-screening and community health worker support
It has been estimated that 520 cases of cervical cancer are linked with socioeconomic disadvantage each year [28]. People living in more socioeconomically disadvantaged areas are less likely to take up the national cervical cancer screening programme [29][30]. Increasing the uptake of national cancer screening programmes is beyond the scope of this evidence brief (see our complementary brief on cervical cancer screening here), but there are effective case finding interventions for women who do not respond to the national screening programme.
Self-sampling may help to find additional cases missed by the national cancer screening programme. A meta-analysis looking at the effectiveness of self-sampling on cervical cancer screening uptake identified 154 studies globally (33% low-income countries) including 482,271 women [31]. Many studies were conducted in marginalised, under-screened populations, although others were looking at the general population. They found that self-sampling almost doubled the probability of cervical cancer screening uptake when compared with samples collected by clinicians, with an opt out approach being most effective. The effect size was greater among previously unscreened women compared to the general population.
Another meta-analysis of 33 studies (26 RCTs in high-income countries, including two in England) similarly found that self-sampling more than doubled screening uptake in screening non-respondents, with greater increases among lower socioeconomic status women [32]. Offering self-testing combined with education through community outreach by health workers had an additional impact, increasing screening uptake by three times in five RCTs of participants from ethnic minority backgrounds or from medically underserved communities. Ethnic minority women and socioeconomically disadvantaged women had higher rates of screening when they had support from a community health worker supervising their self-sampling. Sending reminders to attend clinician delivered screening was also effective in increasing uptake.
Evidence shows that self-sampling shows similar clinical accuracy in detecting cervical pre-cancer as clinician collected samples and addresses many of the barriers to standard cervical screening such as stigma, travel issues to the clinic, taking time off work and arranging childcare which may be beneficial to those from more deprived backgrounds [33][34].
Sun and colleagues considered the cost-effectiveness of different strategies in increasing uptake of cervical cancer screening in underserved women in a systematic review of 17 European studies [30]. Self-sampling as opposed to clinic-based sampling was found to be a preferred and cost-effective add-on to usual screening invitations for underserved women.
Improved coding of GP records
Some patients may receive treatment for a health problem, but not have a diagnosis on their electronic record and therefore miss out on follow-up, such as annual health checks. A 12 month audit in 2018 across 48 practices in East Berkshire identified an additional 6,167 people with hypertension over 12 months through searches for people who had been investigated and received treatment for a condition, but not had a diagnostic code entered into their patient record [35]. Regular audit of electronic health records in general practice to ensure diagnostic codes have been applied correctly and patients are receiving the ongoing management may be a quick and effective way to improve case detection.
2. Opportunistic case finding in the community, workplace or emergency department
Several studies have examined opportunistic case finding in the community, such as BP checks in pharmacies or mobile units, case finding in workplaces or opportunistic case finding when patients attend the emergency department.
Opportunistic community-based case finding
In Derby, 55 volunteers from 17 community groups working with high-risk South Asian, black and deaf communities were provided with blood pressure monitors and trained in delivering blood pressure checks and health education. With a budget of £75,000 over five weeks the volunteers identified 224 people with undiagnosed hypertension who were signposted to community pharmacies for confirmation [16].
Fleming and colleagues (2015) reviewed 73 studies reporting the effectiveness of community-based screening including self-screening for hypertension [36]. The highest proportions of eligible participants screened were through mobile units (range 21%–88%) and pharmacies (range 40%–90%). Roberts and colleagues (2016) looked specifically at reaching diverse groups for the NHS Health Check in Buckinghamshire through community venues compared to general practice [37]. Of 3849 community-based health checks, 11% involved users of South Asian ethnicity (compared to 3% in primary care). Mosques and bus stations were the venues with the broadest reach to underserved groups. An ethnographic study of 20 participants in inner-city Bristol, predominantly from the Afro- Caribbean community, showed that having Health Checks endorsed by trusted community members in lay language supported attendance among disadvantaged groups. Participants indicated that it was their respect for and loyalty to the engagement worker (of similar ethnic background to them) which prompted them to attend the Checks and venues which were both familiar and convenient [38].
Case finding in the workplace
People in low-paid and manual jobs often face being both at high risk of ill health and finding it difficult to take time off to attend preventative health care appointments. Case finding in workplaces potentially offers the opportunity to target low-paid and manual jobs while reducing barriers to preventative care.
A few small-scale studies have explored case finding in workplaces to reach disadvantaged groups. In 2015, Legorreta and colleagues looked at hypertension screening in asymptomatic employees in US workplaces using insurance claims data [39]. Based on 4414 people with high blood pressure, the authors found the African Americans and those on lower incomes were more likely to be diagnosed in the workplace with hypertension compared to white Americans and those on higher incomes. A further US-based study evaluated hypertension case finding in taxi drivers with events at taxi garages, airport holding lots, and app-based driver centres [40]. Most drivers were male, mean age was 47 and half of drivers were not proficient in English. The scheme identified 297 people with undiagnosed hypertension (14% of total and 30% of high risk).
Researchers at the University of Southampton evaluated a case finding initiative on their campus which involved a health questionnaire and BP check [41]. A total of 653 staff and students took part, and the authors found higher rates of hypertension in male manual workers compared to what would have been expected for the age and sex. Finally, Sonkodi and colleagues evaluated hypertension case finding in a salami factory in Hungary which involved a questionnaire and BP check [42]. In total 1012 factory workers were screened, and of the 260 employees with high blood pressure, 100 (39%) were undiagnosed.
Opportunistic case finding in the Emergency Department (ED)
Patients from minority ethnic groups and more socioeconomically disadvantaged areas are more likely to attend EDs and therefore screening for BP with community pharmacy or GP confirmation may be effective for disadvantaged groups [43][44]. Michaud and colleagues (2020) reviewed 10 studies assessing the use of screening for hypertension (measuring BP and making appropriate referrals for diagnostic confirmation) in the emergency department [45]. The authors found that 43.4% of patients with elevated blood pressure during the ED visit were subsequently diagnosed with hypertension.
Additional considerations
Case finding inherently increases primary care workload with more patients requiring diagnosis and management [46]. Formal diagnosis usually requires additional testing. For example, hypertension requires confirmation of diagnosis through either home or ambulatory blood pressure monitoring. A specific challenge with COPD case finding is the quality and availability of diagnostic spirometry, however there is an estimated backlog of 200-250 patients per 500,000 population [47]. Any intervention that will increase the number of people with chronic disease needs additional resources.
Clinicians and patients are generally in favour of case finding. However, barriers include poor knowledge and awareness, fear of diagnoses among patients, increasing workload, difficulty accessing GP appointments and lack of access to diagnostic services [48][49]. Concerns have also been highlighted about potential harm to patients through overdiagnosis [48][50].
What works: Key recommendations
The Grading of Recommendations, Assessment, Development and Evaluations (GRADE) framework has been adopted to grade the quality of the evidence and support recommendations [51].
Recommendations which are supported by large trials will be graded highest whereas those arising from small studies or transferable evidence will be graded lower. The grading should not be interpreted as priority for policy implementation – i.e. some recommendations may have a low GRADE rating but likely to make a substantial population impact.
| Recommendation | Target audience | GRADE certainty |
| Multiple component interventions are needed to identify patients with undiagnosed health problems in various locations and settings. | NHS England, ICBs, PCNs, Trusts, pharmacies and GPs | ⊕ ⊕ ⊕
Moderate |
| Primary care electronic health records should be searched to identify disadvantaged groups who are likely to be undiagnosed with hypertension, diabetes and COPD, rather than relying on opportunistic case finding. | NHS England, ICBs, PCNs and GPs | ⊕ ⊕ ⊕
Moderate |
| Diagnostic coding within primary care records should be audited on a regular basis to ensure people who are being managed for a health problem have a diagnostic code entered. | NHS England, ICBs, PCNs and GPs | ⊕ ⊕ ⊕
Moderate |
| Case finding for COPD using a disease-based questionnaire and hand held flow meter should be considered with additional investment in diagnostic spirometry. | NHS England, ICBs | ⊕ ⊕ ⊕
Moderate |
| Cervical cancer self-screening should be considered for women who do not attend the national screening programme, with the support of community health workers for specific disadvantaged communities. | NHS England, ICBs | ⊕ ⊕ ⊕
Moderate |
| Health checks should be offered in community settings, such as mosques, bus stations and community venues which are familiar to residents. | Local authorities, ICBs | ⊕ ⊕ ⊕
Moderate |
| Consider training key individuals within community organisations to undertake BP checks in underserved communities and commission them to undertake BP checks. | NHS England, ICBs | ⊕
Very low |
| Consider workplace case finding programmes, especially for hypertension and cardiovascular disease. | Local authorities, NHS England, ICBs | ⊕ ⊕
Low |
| Ensure pathways exist for patients who have a high recorded blood pressure in the emergency department to be followed up. | NHS England, Trusts, pharmacies, GP surgeries | ⊕ ⊕ ⊕
Moderate |
| Any new case finding programme should ensure that there is sufficient follow-up diagnostic and management capacity. | NHS England, ICBs | ⊕ ⊕ ⊕
Moderate |
Summary of how this brief was produced
What is the Living Evidence Map on What Works to address health inequalities in primary care?
Using AI-powered software, called EPPI-Reviewer, the Health Equity Evidence Centre has developed a Living Evidence Map of what works to address health inequalities in primary care. The software identifies research articles which examine interventions to address inequalities. The evidence map contains systematic review and umbrella reviews. More information can be found on the Health Equity Evidence Centre website.
Funding
This Evidence Brief has been commissioned by NHS England to support their statutory responsibilities to deliver equitable health care. Policy interventions beyond health care services were not in scope. DL is funded by NIHR ARC North Thames. The views expressed in this publication are those of the author(s) and not necessarily those of NHS England or NIHR.
Suggested citation
Patel A, Painter H, Kuhn I, Gkiouleka A, Holdroyd I, Lamb D, Ford J. ‘What works – Improving case finding of long-term health problems in disadvantaged communities’, Evidence Brief, Health Equity Evidence Centre, 2024.
References
- Quantifying health inequalities in England [Internet]. [cited 2024 Aug 23]
Available from: https://www.health.org.uk/news-and-comment/charts-and-infographics/quantifying-health-inequalities - Coghill N, Garside L, Montgomery AA, Feder G, Horwood J. NHS health checks: a cross- sectional observational study on equity of uptake and outcomes. BMC Health Serv Res. 2018 Apr 3;18(1):238.
- Goff LM. Ethnicity and Type 2 diabetes in the UK. Diabet Med J Br Diabet Assoc. 2019 Aug;36(8):927–38.
- NHS England Digital [Internet]. [cited 2024 Aug 23]. Health Survey for England, 2021 part 2.
Available from: https://digital.nhs.uk/data-and-information/publications/statistical/health-survey-for-england/2021-part-2 - Faculty of Public Health. Differences between screening and diagnostic tests and case finding | Health Knowledge [Internet]. 2017 [cited 2024 Aug 24].
Available from: https://www.healthknowledge.org.uk/public-health-textbook/disease-causation-diagnostic/2c-diagnosis-screening/screening-diagnostic-case-finding - Molokhia M, Ayis DS, Karamanos A, L’Esperance DV, Yousif S, Durbaba S, et al. What factors influence differential uptake of NHS Health Checks, diabetes and hypertension reviews among women in ethnically diverse South London? Cross-sectional analysis of 63,000 primary care records. EClinicalMedicine. 2022 Jul;49:101471.
- Britton M. The burden of COPD in the U.K.: results from the Confronting COPD survey. Respir Med. 2003 Mar;97 Suppl C:S71-79.
- Department of Health (2011). An Outcomes Strategy for Chronic Obstructive Pulmonary Disease (COPD) and Asthma in England. [Internet].
Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216139/dh_128428.pdf - Stone PW, Osen M, Ellis A, Coaker R, Quint JK. Prevalence of Chronic Obstructive Pulmonary Disease in England from 2000 to 2019. Int J Chron Obstruct Pulmon Dis. 2023;18:1565– 74.
- Risk factors for undiagnosed high blood pressure in England – Office for National Statistics [Internet]. [cited 2024 Jul 30].
Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthandwellbeing/articles/riskfactorsforundiagnosedhighbloodpressureinengland/2015to2019 - Bilitou A, Were J, Farrer A, Rabe A, Ming SWY, Haq I, et al. Prevalence and Patient Outcomes of Adult Primary Hypercholesterolemia and Dyslipidemia in the UK: Longitudinal Retrospective Study Using a Primary Care Dataset from 2009 to 2019. Clin Outcomes Res CEOR. 2022 Apr 5;14:189–203.
- Thomas C, Brennan A, Goka E, Squires HY, Brenner G, Bagguley D, et al. What are the cost-savings and health benefits of improving detection and management for six high cardiovascular risk conditions in England? An economic evaluation. BMJ Open. 2020 Sep 10;10(9):e037486.
- Tanner L, Kenny R, Still M, Ling J, Pearson F, Thompson K, et al. NHS Health Check programme: a rapid review update. BMJ Open. 2022 Feb 16;12(2):e052832.
- Community Pharmacy England. Community Pharmacy England. 2024 [cited 2024 Aug 24].
Available from: https://cpe.org.uk/funding-and-reimbursement/nhs-statistics/clinical-services-statistics/ - Hemming K, Ryan R, Gill P, Westerby P, Jolly K, Marshall T. Targeted case finding in the prevention of cardiovascular disease: a stepped wedge cluster randomised controlled trial. Br J Gen Pract J R Coll Gen Pract. 2016 Oct;66(651):e758-767.
- How to address undiagnosed hypertension and health inequalities – Pulse Today [Internet]. [cited 2024 Aug 23].
Available from: https://www.pulsetoday.co.uk/pulse-pcn/how-to-address-undiagnosed-hypertension-and-health-inequalities/ - Kypridemos C, Allen K, Hickey GL, Guzman-Castillo M, Bandosz P, Buchan I, et al. Cardiovascular screening to reduce the burden from cardiovascular disease: microsimulation study to quantify policy options. BMJ. 2016 Jun 8;353:i2793.
- Dirven JAM, Tange HJ, Muris JWM, van Haaren KMA, Vink G, van Schayck OCP. Early detection of COPD in general practice: implementation, workload and socioeconomic status. A mixed methods observational study. Prim Care Respir J J Gen Pract Airw Group. 2013 Sep;22(3):338–43.
- Løkke A, Lange P, Scharling H, Fabricius P, Vestbo J. Developing COPD: a 25 year follow up study of the general population. Thorax. 2006 Nov;61(11):935–9.
- Leidy NK, Martinez FJ, Malley KG, Mannino DM, Han MK, Bacci ED, et al. Can CAPTURE be used to identify undiagnosed patients with mild-to-moderate COPD likely to benefit from treatment? Int J Chron Obstruct Pulmon Dis. 2018 Jun 13;13:1901–12.
- Haroon S, Adab P, Riley RD, Fitzmaurice D, Jordan RE. Predicting risk of undiagnosed COPD: development and validation of the TargetCOPD score. Eur Respir J. 2017 Jun;49(6):1602191.
- Jordan RE, Adab P, Sitch A, Enocson A, Blissett D, Jowett S, et al. Targeted case finding for chronic obstructive pulmonary disease versus routine practice in primary care (TargetCOPD): a cluster-randomised controlled trial. Lancet Respir Med. 2016 Sep;4(9):720–30.
- Adab P, Jordan RE, Fitzmaurice D, Ayres JG, Cheng KK, Cooper BG, et al. Case-finding and improving patient outcomes for chronic obstructive pulmonary disease in primary care: the BLISS research programme including cluster RCT [Internet]. Southampton (UK): NIHR Journals Library; 2021 [cited 2024 Aug 23].
Available from: http://www.ncbi.nlm.nih.gov/books/NBK575161/ - Haroon S, Adab P, Dickens A, Sitch A, Rai K, Enocson A, et al. Impact of COPD case finding on clinical care: a prospective analysis of the TargetCOPD trial. BMJ Open. 2020;
- Jordan R, Adab P, Sitch AJ, Enocson A, Blissett DB, Jowett S, et al. Targeted case finding for chronic obstructive pulmonary disease versus routine practice in primary care (Target- COPD): a cluster-randomised controlled trial. Lancet Respir Med. 2016;
- Mountain R, Kim D, Johnson KM. Budget impact analysis of adopting primary care-based case detection of chronic obstructive pulmonary disease in the Canadian general population. CMAJ Open. 2023;
- Chen Q, Fan Y, Huang K, Li W, Geldsetzer P, Bärnighausen T, et al. Cost-effectiveness of population-based screening for chronic obstructive pulmonary disease in China: a simulation modeling study. Lancet Reg Health West Pac. 2024 May;46:101065.
- Cancer Research UK [Internet]. 2015 [cited 2024 Aug 28]. Cervical cancer statistics
Available from: https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/cervical-cancer - Cadman L, Wilkes S, Mansour D, Austin J, Ashdown-Barr L, Edwards R, et al. A randomized controlled trial in non-responders from Newcastle upon Tyne invited to return a self-sample for Human Papillomavirus testing versus repeat invitation for cervical screening. J Med Screen. 2015 Mar;22(1):28–37.
- Bardou Marc, et al. A systematic review of the cost-effectiveness of interventions to increase cervical cancer screening among underserved women in Europe. Eur J Health Econ [Internet]. 2023;
Available from: https://link.springer.com/article/10.1007/s10198-023-01627-1 - Di Gennaro G, Licata F, Trovato A, Bianco A. Does self-sampling for human papilloma virus testing have the potential to increase cervical cancer screening? An updated meta-analysis of observational studies and randomized clinical trials. Front Public Health. 2022;10:1003461.
- Yeh Ping Teresa, Kennedy Caitlin E, Vuyst Hugo de, Narasimhan Manjulaa. Self-sampling for human papillomavirus (HPV) testing: a systematic review and meta-analysis. BMJ Glob Health. 2019;4(3):e001351.
- Arbyn M, Verdoodt F, Snijders PJF, Verhoef VMJ, Suonio E, Dillner L, et al. Accuracy of human papillomavirus testing on self-collected versus clinician-collected samples: a meta- analysis. Lancet Oncol. 2014 Feb 1;15(2):172–83.
- Aimagambetova G, Atageldiyeva K, Marat A, Suleimenova A, Issa T, Raman S, et al. Comparison of diagnostic accuracy and acceptability of self-sampling devices for human Papillomavirus detection: A systematic review. Prev Med Rep. 2024 Feb 1;38:102590.
- NICE [Internet]. NICE; [cited 2024 Aug 23]. Systematic case finding of people with hypertension.
Available from: https://www.nice.org.uk/sharedlearning/systematic-case-finding-of-people-with-hypertension - Fleming S, Atherton H, McCartney D, Hodgkinson J, Greenfield S, Hobbs FDR, et al. Self-Screening and Non-Physician Screening for Hypertension in Communities: A Systematic Review. Am J Hypertens. 2015 Nov;28(11):1316–24.
- Roberts DJ, de Souza VC. A venue-based analysis of the reach of a targeted outreach service to deliver opportunistic community NHS Health Checks to ‘hard-to-reach’ groups. Public Health. 2016 Aug;137:176–81.
- Riley R, Coghill N, Montgomery A, Feder G, Horwood J. The provision of NHS health checks in a community setting: an ethnographic account. BMC Health Serv Res. 2015 Dec 10;15(1):546.
- Legorreta AP, Schaff SR, Leibowitz AN, van Meijgaard J. Measuring the Effects of Screening Programs in Asymptomatic Employees: Detection of Hypertension Through Worksite Screenings. J Occup Environ Med. 2015 Jun;57(6):682
- Narang B, Mirpuri S, Kim SY, Jutagir DR, Gany F. Lurking in plain sight: Hypertension awareness and treatment among New York City taxi/for‐hire vehicle drivers. J Clin Hypertens. 2020 May 21;22(6):962–9.
- Getliffe KA, Crouch R, Gage H, Lake F, Wilson SL. Hypertension awareness, detection and treatment in a university community: results of a worksite screening. Public Health. 2000 Sep;114(5):361–6.
- Sonkodi B, Fodor JG, Ábrahám G, Légrády P, Ondrik Z, Lencse G, et al. Hypertension screening in a salami factory: a worksite hypertension study. J Hum Hypertens. 2004 Aug;18(8):567–9.
- Inequalities in Accident and Emergency department attendance, England – Office for National Statistics [Internet]. [cited 2024 Jul 30].
Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthcaresystem/articles/inequalitiesinaccidentandemergencydepartmentattendanceengland/march2021tomarch2022 - The Relationship Between Poverty And NHS Services | The King’s Fund [Internet]. [cited 2024 Aug 23].
Available from: https://www.kingsfund.org.uk/insight-and-analysis/long-reads/relationship-poverty-nhs-services - Michaud A, Lamarre-Cliche M, Vadeboncoeur A, Cloutier L. Screening for hypertension in adults during emergency department consultation: a systematic review. Eur J Emerg Med Off J Eur Soc Emerg Med. 2020 Jun;27(3):178–85.
- Lay-Flurrie SL, Sheppard JP, Stevens RJ, Mallen C, Heneghan C, Hobbs FR, et al. Impact of changes to national guidelines on hypertension-related workload: an interrupted time series analysis in English primary care. Br J Gen Pract [Internet]. 2020 Dec 17 [cited 2024 Jul 30];
Available from: https://bjgp.org/content/early/2021/03/22/bjgp21X714281 - Lay-Flurrie SL, Sheppard JP, Stevens RJ, Mallen C, Heneghan C, Hobbs FR, et al. Impact of changes to national guidelines on hypertension-related workload: an interrupted time series analysis in English primary care. Br J Gen Pract J R Coll Gen Pract. 2021 Apr;71(705):e296–302.
- Haroon S, Jordan RE, Fitzmaurice DA, Adab P. Case finding for COPD in primary care: a qualitative study of the views of health professionals. Int J Chron Obstruct Pulmon Dis. 2015 Aug 28;10:1711–8.
- Enocson A, Jolly K, Jordan RE, Fitzmaurice DA, Greenfield S, Adab P. Case-finding for COPD in primary care: a qualitative study of patients’ perspectives. Int J Chron Obstruct Pulmon Dis. 2018 May 17;13:1623–32.
- Rose D, Ray E, Summers RH, Taylor M, Kruk H, North M, et al. Case-finding for COPD clinic acceptability to patients in GPs across Hampshire: a qualitative study. Npj Prim Care Respir Med. 2021;
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso- Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008 Apr 24;336(7650):924–6.