What works: Improving access, uptake and optimisation of behavioural interventions in the health care setting to better meet the needs of disadvantaged groups

Tackling chronic disease risk factors requires a systemic approach that addresses the structural barriers that disadvantaged groups face in managing their health. In this evidence brief, we focus on how health care services, as part of this system, can improve behavioural interventions aiming to tackle chronic disease risk factors like smoking, obesity, or hypertension, so that they better address the needs and preferences of disadvantaged groups.
What works- Improving access, uptake and optimisation of behavioural interventions in the health care setting to better meet the needs of disadvantaged groups[PDF 254kb]
Download documentSummary
Tackling chronic disease risk factors requires a systemic approach that addresses the structural barriers that disadvantaged groups face in managing their health. In this evidence brief, we focus on how health care services, as part of this system, can improve behavioural interventions aiming to tackle chronic disease risk factors like smoking, obesity, or hypertension, so that they better address the needs and preferences of disadvantaged groups.
Based on HEEC living evidence maps, a Medline search for review studies on behavioural interventions and snowball searching, we screened 1796 studies and extracted data from 153 reviews.
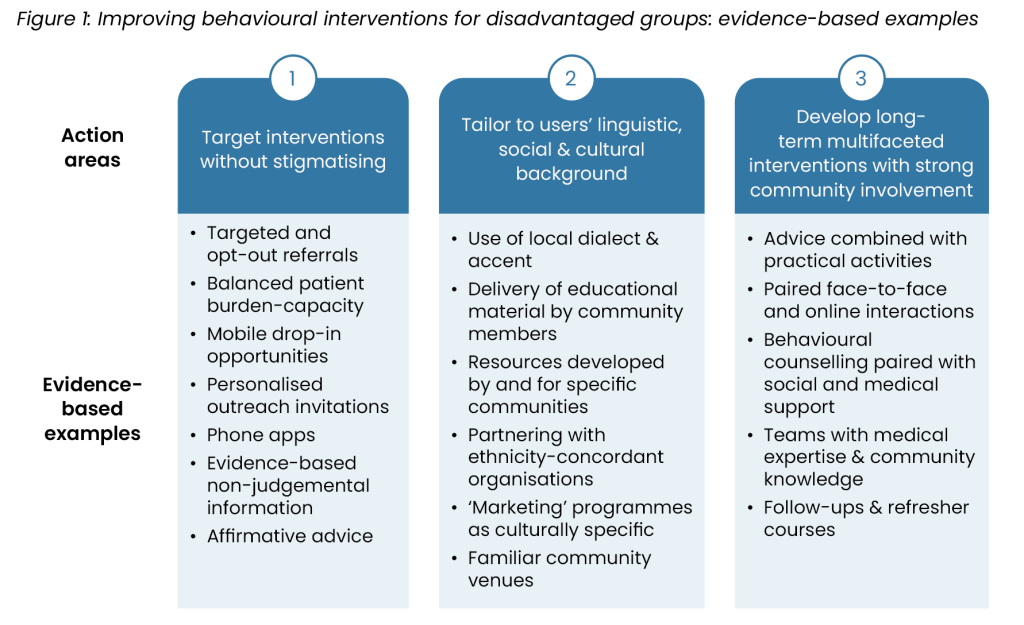
Improving access, uptake and optimisation of behavioural interventions for disadvantaged groups requires a flexible approach, as no single solution fits all. Effective strategies are usually locally focused, non-stigmatising, and adapted to the community’s linguistic, cultural, and social needs. These interventions work best when delivered over time in a multifaceted way combined with strong community involvement.
Current challenges
There is a consensus that poor diet, smoking or vaping, substance misuse, and sedentary lifestyle are risk factors for chronic conditions like Type 2 diabetes, cardiovascular and respiratory diseases [1]. Evidence shows that often these factors are more prevalent among people living in socioeconomically deprived areas, some people of ethnic minority backgrounds, and individuals experiencing multiple intersectional disadvantage [2][3]. In the last couple of decades, increasingly these factors are being described as unhealthy or health damaging behaviours – often disconnected from the socioeconomic and cultural drivers that enable them – and are therefore understood as modifiable and subject to change through behavioural or lifestyle interventions [4][5][6].
Behavioural or lifestyle interventions are interventions which aim to improve health by encouraging changes in behaviour. Most often they focus on people’s diet, smoking and drinking habits and physical activity (PA). They are often complex interventions with several interactive components like provision of health education, behavioural counselling or cognitive behavioural therapy (CBT), and practical components like participation in exercise programmes or cooking classes [7]. They are delivered in different formats and settings ranging from online courses to group activities and individual one-to-one counselling sessions.
Evidence shows that among the general population, behavioural interventions are overall effective in reducing body weight and body mass index (BMI), increasing fruit and vegetable consumption and physical activity and reducing risk of chronic conditions and all-cause mortality [8][9][10][11][12][13]. Further, behavioural support or counselling has been found to increase smoking cessation rates especially for people who do not receive pharmacotherapy [14] and reduce unhealthy alcohol consumption [15].
However, additional evidence shows that behavioural strategies are differentially effective across different population groups [16]. People who are socially and financially secure tend to access and benefit more from such interventions because of their increased capacity (material, psychological, and social) to make behavioural changes compared to socially and economically disadvantaged individuals [17]. Therefore, behavioural approaches, despite their potential to improve general population health, often maintain or even widen inequalities in health care and health outcomes between population groups [18]. As the NICE guideline on individual approaches in behaviour change stresses, equity audits are required to ensure that behaviour change strategies do not increase health inequalities [19]. Health care services – while limited in their capacity to address structural barriers prohibiting disadvantaged groups from adopting healthier practices – need to consider these barriers when designing and delivering behavioural interventions to ensure the potential benefits reach those who need them the most.
In this brief, we review evidence on improving access, uptake and optimisation of behavioural inventions for disadvantaged groups in health care settings. The root causes of inequalities in chronic disease risk factors extend beyond health care. A systemic approach is essential – one that addresses the social determinants of health and the support gaps that disadvantaged groups face in accessing care and managing their health [18][19][20].
General criteria to consider when specifying factors as ‘modifiable’ in the context of health and disease outcomes
- Measurability: the factor can be measured.
- Potential for change: there is potential for change in the quantity and intensity of the modifiable factor at individual or/and
population level. - Modifiable causes: the drivers of the risk factor are modifiable themselves.
- Plausibility: the risk factor can be considered as a plausible cause of the outcome of interest.
- Empirical evidence of effect: there’s empirical evidence of the factor’s direct effect on health outcomes.
Summary of evidence
For the purposes of this brief, we defined behavioural interventions as sets of behavioural strategies aiming to improve an individual’s health by encouraging behavioural changes related with diet, physical activity, smoking habits, or alcohol consumption and/or with chronic disease selfmanagement like blood-pressure monitoring or medication adherence. We searched for relevant review studies through the Living Evidence Maps of the Health Equity Evidence Centre (HEEC), a Medline search and snowball searching. Out of 1796 studies screened, we included 153 reviews.
The reviews focused on behavioural interventions targeted to improve health or health care related outcomes among disadvantaged groups, or to reduce inequalities in such outcomes between groups. They discussed interventions delivered in diverse settings with a health care services component and focused on intervention impacts or enablers as reported by service users. Additionally, we integrated transferable evidence from a realist [16] and an integrative [21] review of interventions decreasing health inequalities through general practice (GP) published in 2023.
The reviewed evidence covered a wide range of localities, settings, interventions, targeted groups, and condition related outcomes including diabetes, blood pressure and hypertension, asthma, and chronic obstructive pulmonary disease (COPD), and risk factors including body weight and Body Mass Index (BMI), smoking rates, physical activity, and alcohol consumption. There is no single or set of specific interventions that can guarantee increased access, uptake and optimisation of behavioural interventions. Rather, the most effective interventions vary across different contexts and settings but have overlapping characteristics across three key areas. They tend to be 1) targeted at specific populations in non-stigmatising ways, 2) tailored to users’ linguistic, cultural and social background, and 3) delivered over long periods of time employing multiple components and strong community involvement. In figure 1, we organise the most important findings across these three key areas.
1. Target efforts at disadvantaged groups without further stigmatising them
A systematic review of the impact of chronic disease self-management support interventions on health equity gaps showed that people of lower socioeconomic status are less likely to participate in relevant programmes [22]. The authors reviewed 19 studies of moderate to good quality from different countries. They found that programmes with targeted recruitment and retention strategies, e.g., through referrals rather than self-selection, are more likely to improve participation. Further, interventions which addressed users’ social context and did not add to their workload were more likely to lead to positive clinical outcomes among disadvantaged groups compared to interventions focusing on self-efficacy. Based on their findings, they recommended the Cumulative Complexity model, founded on patient burden-capacity balance, as a useful framework to inform clinical practice [23].
Literature focusing on smoking cessation interventions in the UK also supports a targeted approach. A systematic review [24] and equity analysis of the impact of specialist and primary care stop smoking support (SSS) on socioeconomic inequalities is an example. It showed that GP brief interventions were equity-positive in terms of identifying disadvantaged smokers and encouraging them to quit. Smokers with lower socioeconomic status were more likely to have their smoking status recorded and be offered brief advice or SSS referral and cessation medication. A review of studies across Europe highlighted that this targeted approach in the UK appears to reduce inequalities in access, compensating for lower quit rates to produce a positive overall equity impact on smoking prevalence [25]. Recent findings add that mobile drop-in SSS might be an effective way of reaching more disadvantaged smokers from routine or manual occupations, and those who have not previously accessed standard support. In a programme conducted in Nottingham city, mobile SSS smokers (n=811) were more likely to be routine or manual workers (33.3% vs 27.2%, p=0.002) and to be first-time SSS users (67.8% vs 59.3%, p<0.001) compared with smokers accessing the standard SSS scheme (n=1856) [26].
Targeted recruitment requires a good understanding of the individuals or groups at higher risk who are often marginalised within health care services. An integrative review of interventions that can reduce inequalities in and through primary care demonstrated that identifying the group(s) harmed by health inequalities using a sensitive localised approach is the key first step for the delivery of equitable care (see more at HEEC website) [21]. A scoping review of recruitment strategies for engaging adults in PA found limited evidence about the suitability of recruitment approaches for those experiencing barriers to PA, particularly those from culturally and linguistically diverse populations, older people, or people from low socioeconomic backgrounds. However, the authors highlighted that in all the reviewed studies (n=9) successful recruitment was subject to ‘knowing your audience’ [27].
Understanding the lived experience of those who face barriers in accessing interventions can assist in undertaking recruitment in acceptable and practical ways. For example, health promotion interventions targeted to unemployed people have better participation rates when participation is voluntary [28], and smoking cessation interventions with an ‘opt-out’ referral system are more acceptable among pregnant smokers [29]. Similar conclusions emerge from studies on influences on NHS health check behaviours. They show that people are more likely to attend checks if they are reassured and feel comfortable (e.g., through outreach services at familiar venues) [30]. Subsequently they can change their behaviours when they can understand the purpose of the checks as an opportunity to be proactive regarding their CVD risk [31].
Stigma as a barrier to service engagement
A series of qualitative reviews discuss how for disadvantaged groups stigma is a barrier to engagement with health care services and interventions, especially when the latter focus on behaviour changes and risk factors. Medical narratives that primarily focus on treatment tend to understand individual behaviours as the causes of risk factors such as obesity or smoking. The underlying assumptions are that behaviour is the outcome of informed choice and that individuals are independent agents [17]. Accordingly behavioural interventions often focus on the provision of information material which is assumed to help individuals make the right choices for their health. When this does not work, individuals are increasingly blamed for ‘failing’ [20].
Most relevant studies discuss stigma related with smoking or obesity due to the normalisation of stereotypes that render smokers and obese people as people of weak character, or threats to their children, and associate them with more negative stereotypes like the ‘chav’ in the UK or the ‘welfare queen’ in the US [17][32][33]. As the stereotypes indicate, smoking and weight stigma intersect with socioeconomic status, gender and ethnicity. Therefore, many qualitative studies have focused on women with low socioeconomic status and/or from ethnic minority backgrounds.
A review of 23 qualitative studies from Western developed countries showed that women are likely to hide their smoking from health professionals, especially if they are pregnant, to avoid potentially stigmatising remarks. Further, they express negative views of medical professionals, describing them as paternalistic and overly reliant on brochures and lectures [35]. A UK study focusing on the willingness of smokers to use NHS SSS also addressed stigma as a barrier to use for women, especially if they are pregnant, to avoid feeling judged. They recommended that interventions are more likely to help individuals overcome such barriers if they include personalised outreach invitations and phone apps [29].
Similarly, a meta-synthesis of 46 qualitative studies focused on factors influencing weight management during pregnancy in women who are overweight or obese. It showed that women endure stigmatisation by the community and health care professionals which negatively affects their physical and mental health outcomes. In a total sample of 910 women, providing evidence-based information and counselling in a sensitive, non-judgemental way emerged as a prominent component of effective weight management interventions [36]. These findings highlight the need for trained and empowered health care professionals who feel confident to discuss weight with patients in an affirmative way using the right concepts and words (e.g., weight instead of fat or obese) and have sufficient knowledge of available referral pathways for support [37].
2. Tailor programmes to service users’ languages, values and cultural practices
Ensuring that interventions, whether face-to-face or digital, align with users’ language and cultural background is key to person-centred care but can also benefit uptake and outcomes among disadvantaged groups including people from ethnic minority backgrounds, linguistically diverse groups, and groups with low socioeconomic status.
A systematic review and meta-analysis of 31 studies focused on interventions to improve the quality of diabetes care in African Americans. It showed that programmes, which mainly included culturally adapted diabetes self-management education, reduced the percentage of Hemoglobin A1c (HbA1c) by 0.8% [38]. Another meta-analysis of 12 studies with 1495 participants also showed that people from ethnic minority backgrounds benefit more from culturally tailored diabetes education when compared with usual care. The effect of intervention was greatest when HbA1c level was measured at 6 months (−0.41; 95% confidence interval, −0.61 to −0.21).
A systematic review and meta-analysis of 58 studies of tailored education for culturally and linguistically diverse (CALD) groups revealed that culturally appropriate services had short-term (≤ 6 months) and medium-term (6 to 12 months) impact on obesity, cholesterol and HbA1c [40]. Cultural tailoring and linguistic adaptation were differentially defined and implemented across studies. A systematic review of 74 studies focused on community based culturally tailored education for black communities with chronic conditions. It highlighted that impactful linguistic strategies did not involve translated material but rather included using the local dialect and accent of the target community and having black community members delivering education material [41].
The study revealed a wide range of additional tailoring strategies which included:
- Peripheral strategies, e.g., ‘marketing’ the programmes as culturally specific for African Americans.
- Evidential strategies which used resources developed for the target communities, e.g., discussion of race-specific health strategies such as foot care for people with dark skin tones.
- Constituent-involving strategies, e.g., incorporating lay individuals or key celebrities in information sharing and/or partnering with ethnicity-concordant organisations that served black communities.
- Socio-cultural strategies, e.g., dance classes, use of cultural recipes, involvement of family members.
Location was also stressed as an important factor in tailoring interventions to communities’ needs which complements an additional systematic review of tailoring methods and their effectiveness among people from black ethnicities with diabetes [42]. The review showed there are four domains of tailoring (location, facilitators, messaging and language). Most interventions tailored to location and facilitators, but less to messaging and language. Seven out of 16 studies incorporated more than two domains of cultural adaptation, and four found significant difference between groups in HbA1c, weight and diabetes knowledge. Overall, interventions that tailored to all four domains showed greater success than those only tailoring to one.
Cultural tailoring is relevant to digital interventions as well as shown by a realist review of digital interventions for CVD among South Asian and black minority ethnic groups [43]. Based on 15 studies, the authors found that what makes interventions relatable and acceptable differs across ethnic groups. For example, people from the South Asian ethnic group valued learning from family, and people from the African American ethnic group prioritised community, such as learning health information from their peers. Digital health interventions that were positively reviewed by participants across all ethnic groups included those that provided education modules which were easy to understand.
A further discussion on the importance of the cultural domain in the design and delivery of equitable care can be found in HEEC website and in the complementary HEEC evidence briefs on improving health literacy among disadvantaged groups, and community engagement and empowerment to address health inequalities.
3. Develop long-term multifaceted interventions with strong community involvement
Behavioural interventions are often complex with multiple interrelated components, (e.g., outreach activities and behavioural counselling [44]), formats (e.g., face-to-face discussions and online applications [45]), or professionals (e.g., licensed health care professionals with non-medical professionals [46]). Overall, the evidence does not offer sufficient guidance in terms of which of these components are more effective in improving uptake and effectiveness among disadvantaged groups. This is due to the great diversity of targeted groups, interacting nature of different components, and interventions being subject to their context [21]. It is also due to limitations of the reviewed studies which in their vast majority compare complex interventions with usual care instead of different interventions or different components.
Effective interventions for disadvantaged groups often include training staff [47] to support chronic disease management in a clear and supportive way [48]. Weight management interventions with positive impacts usually include a combination of 1) environmental enhancements (i.e., related with housing, transportation, or access to recreational facilities), 2) acceptance-based enhancements (e.g., a body-positive approach: having or showing acceptance and appreciation of all body types [49]) and 3) a combination of advice (e.g., on healthy food options) with some practical activities (e.g., walking) [50]. Combined diet and PA promotion programmes are also effective in decreasing diabetes incidence and improving cardiometabolic risk factors for patients at increased risk [51], especially people who are unemployed. They are also effective for people from minority ethnic backgrounds with higher diabetes prevalence when they are culturally tailored [48]. Finally, findings regarding smoking cessation show that more effective approaches combine behavioural counselling, pharmacological support and in-person or phone follow-ups to facilitate nicotine replacement and address difficulties. Findings are promising also for people from ethnic minority and migration backgrounds [52][53].
Community engagement in programme design and delivery is also key for the effectiveness of interventions (see more in the HEEC Community Engagement and Empowerment Evidence Brief). Here, we focus specifically on behavioural interventions. Systematic reviews support involving members of the target community in design and delivery to ensure the cultural and linguistic tailoring of interventions to communities’ needs and preferences [41][54]. Additional evidence suggests that trained community health workers (CHWs) or peer supporters/leaders can effectively deliver behavioural interventions with positive impacts among low-income, underserved, and racial and ethnic minority groups [55][56][57]. For example, after reviewing 17 studies, Rawal and colleagues found that lifestyle interventions using either CHWs or peer supporters or a combination have modest effectiveness in the management of type 2 diabetes among people from ethnic minority or migrant backgrounds. Their meta-analyses showed that interventions were associated with a small but statistically significant reduction in HbA1c (−0.18%; 95% CI −0.32% to −0.04%). However, they were not able to produce definite conclusions about potential differences in effectiveness between CHW and peer-led programmes [58].
WHO definition of Community Health Workers: members of communities who are supported by the health system but not necessarily a part of its organisation and have shorter training than professional workers [59].
Further, a study on diabetes self-management education showed that when participants were assigned to a team of people, rather than an individual, there was a greater HbA1C reduction (-0.295%; 99% CI 0.505, −0.085) [46]. The authors concluded that combining clinical expertise of professionals with community members is likely to improve health outcomes in high-risk populations. Additionally, a meta-analysis of six studies including 1280 participants from ethnic minority backgrounds showed a significant improvement in HbA1c level at 12 months follow-up, with a mean weighted difference of 0.5% (95% CI 0.31–0.68) in the CHW group [60].
Longer duration is another key aspect of effective behavioural interventions. Most studies we reviewed focused on short (<6 months) to medium term (6-12 months) impacts, highlighting the need for longer-term approaches for positive changes to be sustained. A systematic review and meta-analysis of studies on diabetes self-management education in people from Latino backgrounds found that the greatest reduction in HbA1C was in studies that were ≤ 6 months (−0.274%; 99% CI −0.510, −0.039). Based on adult learning theories, the authors suggested that the effect of new information fades after about 6 months leading to the relapse of old behaviours within a year; demonstrating the need for ongoing support to the educational format [46].
Follow-ups and refresher courses were suggested also by Paul and colleagues who reviewed health promotion and PA interventions for unemployed people [28]. With data from 34 studies, they found that within the upper limit of about 9 weeks, longer training programmes were more successful than shorter, and within the upper limit of 40- hour contact time, higher intensity training was more promising than lower intensity. Similar findings emerged in two systematic reviews of the effectiveness of interventions at reducing socioeconomic inequalities in obesity. They showed that tailored PA and weight management interventions delivered in primary care or community settings have short- to medium-term impacts highlighting the need for follow up and long-term evaluation [61]. Finally, sustained implementation is supported in a review of socioeconomic inequality impacts of chronic disease self-management. Based on 19 studies from different countries, the authors concluded that although such interventions can impact groups with lower socioeconomic status differently, more individualised treatment over longer time periods (6-12 months) tend to be more effective in reducing inequalities [22].
Limitations
This evidence brief covered existing international review articles identified through the HEEC evidence maps, a search on Medline for studies published from 2018, and snowball searching. While we are confident that we have captured the breadth of the published academic evidence, it is likely that we have not integrated key primary studies that may have offered deeper insights to interventions’ characteristics. The majority of evidence reviewed concerns the impact of complex multicomponent interventions in comparison to usual care. The studies did not compare different intervention strategies with each other or different intervention components. They did not address potential differential impacts of interventions across different groups. This means that the findings, even when they describe positive intervention impacts, may have different impacts in different contexts or population groups and do not allow for direct generalisations.
What works: Key recommendations
The Grading of Recommendations, Assessment, Development and Evaluations (GRADE) [32] framework has been adopted to grade the quality of the evidence and support recommendations.
| Recommendation | Target audience | GRADE certainty |
| Acknowledge in policy and practice the structures and social determinants that lead to disadvantaged groups being more susceptible to chronic disease risk factors. | NHS England, ICBs, PCNs, trusts, pharmacies, local authorities and GPs | ⊕ ⊕ ⊕
Moderate |
| Use local knowledge to identify underserved groups with unmet needs and target with tailored and empowering programmes. | NHS England, ICBs, PCNs, local authorities | ⊕ ⊕ ⊕
Moderate |
| Co-design and deliver interventions with community members and develop partnerships that combine clinical expertise and community knowledge. | NHS England, ICBs, PCNs, local authorities | ⊕ ⊕ ⊕
Moderate |
| Tackle weight and smoking stigma through agreed language, educational material and training for staff and community members. | NHS England, ICBs, local authorities | ⊕ ⊕
Low |
| Ensure programmes are culturally tailored through delivery in familiar and convenient locations, local partnerships, and upskilling health and care staff. | NHS England, ICBs, PCNs, trusts, pharmacies, local authorities and GPs | ⊕ ⊕ ⊕
Moderate |
| Recruit frontline health and care staff who can speak a range of languages and dialects according to local need. | NHS England, ICBs, PCNs, trusts, pharmacies, local authorities and GPs | ⊕ ⊕
Low |
| Develop programmes that provide multiple contact opportunities and ongoing support across sustained periods. | NHS England, ICBs, PCNs, trusts, pharmacies, local authorities and GPs | ⊕ ⊕ ⊕
Moderate |
How this brief was produced
Using AI-powered software called EPPI-Reviewer, the Health Equity Evidence Centre has developed a Living Evidence Map of what works to address health inequalities in primary care. The software identifies research articles that examine interventions to address inequalities. The evidence map contains systematic reviews, umbrella reviews. More information can be found on the Health Equity Evidence Centre website.
This Evidence Brief has been commissioned by NHS England to support their statutory responsibilities to deliver equitable health care. Policy interventions beyond health care services were not in scope. DL is funded by NIHR ARC North Thames. The views expressed in this publication are those of the author(s) and not necessarily those of NHS England or NIHR.
Funding
This Evidence Brief has been commissioned by NHS England to support their statutory responsibilities to deliver equitable health care. Policy interventions beyond health care services were not in scope. DL is funded by NIHR ARC North Thames. The views expressed in this publication are those of the author(s) and not necessarily those of NHS England or NIHR.
Suggested citation
Gkiouleka A, Harasgama S, Pearce H, Kuhn I, Dehn Lunn A, Torabi P, Birch J, Lamb D, Vodden A, Engamba S, Ford J. ‘What works – Improving access, uptake and optimisation of behavioural interventions in the health care setting to better meet the needs of disadvantaged groups’, Evidence Brief, Health Equity Evidence Centre, 2024
References
- Everest G, Marshall L, Fraser C, Briggs A. Addressing the leading risk factors for ill health
- Non communicable diseases [Internet]. [cited 2024 Aug 21]
Available from: https://www.who.int/news-room/fact-sheets/detail/%20noncommunicable-diseases - Marteau TM, Rutter H, Marmot M. Changing behaviour: an essential component of tackling health inequalities. BMJ. 2021 Feb 10;372:n332.
- Adams ML, Grandpre J, Katz DL, Shenson D. The impact of key modifiable risk factors on leading chronic conditions. Preventive Medicine. 2019 Mar 1;120:113–8.
- Alwan NA, Stannard S, Berrington A, Paranjothy S, Hoyle RB, Owen RK, et al. Risk factors for ill health: How do we specify what is ‘modifiable’? PLOS Global Public Health. 2024 Mar 4;4(3):e0002887
- Kandt J. Social practice, plural lifestyles and health inequalities in the United Kingdom. Sociology of Health & Illness. 2018;40(8):1294– 311.
- Bradley T, Campbell E, Dray J, Bartlem K, Wye P, Hanly G, et al. Systematic review of lifestyle interventions to improve weight, physical activity and diet among people with a mental health condition. Systematic Reviews. 2022 Sep 9;11(1):198.
- Galani C, Schneider H. Prevention and treatment of obesity with lifestyle interventions: review and meta-analysis. International journal of public health. 2007;52:348–59.
- Foster C, Hillsdon M, Thorogood M, Kaur A, Wedatilake T. Interventions for promoting physical activity – Foster, C – 2005 | Cochrane Library. [cited 2024 Aug 21]
Available from: https://www.cochranelibrary.%20com/cdsr/doi/10.1002/14651858.CD003180.pub2/full - Rees K, Dyakova M, Ward K, Thorogood M, Brunner E. Dietary advice for reducing cardiovascular risk – Rees, K – 2013 | Cochrane Library. [cited 2024 Aug 21]
Available from: https://www.cochranelibrary.%20com/cdsr/doi/10.1002/14651858.CD002128.pub4/full - Ma C, Avenell A, Bolland M, Hudson J, Stewart F, Robertson C, et al. Effects of weight loss interventions for adults who are obese on mortality, cardiovascular disease, and cancer: systematic review and meta-analysis. bmj. 2017;359.
- Kritchevsky SB, Beavers KM, Miller ME, Shea MK, Houston DK, Kitzman DW, et al. Intentional Weight Loss and All-Cause Mortality: A Meta-Analysis of Randomized Clinical Trials. PLOS ONE. 2015 Mar 20;10(3):e0121993.
- LeBlanc ES, Patnode CD, Webber EM, Redmond N, Rushkin M, O’Connor EA. Behavioral and Pharmacotherapy Weight Loss Interventions to Prevent Obesity-Related Morbidity and Mortality in Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2018 Sep 18;320(11):1172–91.
- Hartmann-Boyce J, Livingstone-Banks J, Ordóñez-Mena JM, Fanshawe TR, Lindson N, Freeman SC, et al. Behavioural interventions for smoking cessation: an overview and network meta‐analysis – Hartmann-Boyce, J – 2021 | Cochrane Library. [cited 2024 Aug 21
Available from: https://www.cochranelibrary.com/cdsr/%20doi/10.1002/14651858.CD013229.pub2/full - O’Connor EA, Perdue LA, Senger CA, Rushkin M, Patnode CD, Bean SI, et al. Screening and Behavioral Counseling Interventions to Reduce Unhealthy Alcohol Use in Adolescents and Adults: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2018 Nov 13;320(18):1910–28.
- Gkiouleka A, Wong G, Sowden S, Bambra C, Siersbaek R, Manji S, et al. Reducing health inequalities through general practice. The Lancet Public Health. 2023;8(6):e463–72.
- Adler NE, Stewart J. Reducing Obesity: Motivating Action While Not Blaming the Victim. The Milbank Quarterly. 2009;87(1):49–70.
- Williams O, Fullagar S. Lifestyle drift and the phenomenon of ‘citizen shift’ in contemporary UK health policy. Sociology of Health & Illness. 2019;41(1):20–35
- Recommendations | Behaviour change: individual approaches | Guidance | NICE [Internet]. NICE; 2014 [cited 2024 Aug 27]
Available from: https://www.nice.org.uk/guidance/ph49/chapter/%20Recommendations#recommendation-7-use-proven-behaviour-%20change-techniques-when-designing-interventions - Hiam L, Klaber B, Sowemimo A, Marmot M. NHS and the whole of society must act on social determinants of health for a healthier future. bmj. 2024;385.
- Jackson B, Ariss S, Burton C, Coster J, Reynolds J, Lawy T. The FAIRSTEPS Study: Framework to Address Inequities in pRimary care using STakEholder PerspectiveS—short report and user guidance. 2023.
- Hardman Ruth, Begg Stephen, Spelten Evelien. What impact do chronic disease self-management support interventions have on health inequity gaps related to socioeconomic status: a systematic review. BMC Health Services Research [Internet]. 2020;20(1)
Available from: https://explore.openalex.org/works/W3012662296 - Shippee ND, Shah ND, May CR, Mair FS, Montori VM. Cumulative complexity: a functional, patient-centered model of patient complexity can improve research and practice. Journal of Clinical Epidemiology. 2012 Oct 1;65(10):1041–51.
- Smith Caroline E, Hill Sarah E, Amos Amanda. Impact of specialist and primary care stop smoking support on socioeconomic inequalities in cessation in the United Kingdom: a systematic review and national equity analysis. Addiction. 2020;115(1):34–46.
- Brown Tamara, Platt Stephen, Amos Amanda. Equity impact of European individual-level smoking cessation interventions to reduce smoking in adults: a systematic review. European Journal of Public Health. 2014 Aug;24(4):551–6.
- Venn A, Dickinson A, Murray R, Jones L, Li J, Parrott S, et al. Effectiveness of a mobile, drop-in stop smoking service in reaching and supporting disadvantaged UK smokers to quit. Tobacco Control. 2016 Jan 1;25(1):33–8.
- Mackenzie-Stewart R, De Lacy-Vawdon C, Murphy N, Smith BJ. Engaging adults in organized physical activity: a scoping review of recruitment strategies. Health Promotion International. 2023 Jun 1;38(3):daad050.
- Paul Karsten Ingmar, Hollederer Alfons. The Effectiveness of Health-Oriented Interventions and Health Promotion for Unemployed People-A Meta-Analysis. International journal of environmental research and public health [Internet]. 2023;20(11).
Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&%20D=med24&NEWS=N&AN=37297632 - Latif Asam, Murray Rachel L, Waters Claire, Leonardi-Bee Jo. Understanding willingness to access and experiences of NHS Stop Smoking Services: a qualitative systematic review with meta-aggregation synthesis. Public health. 2021;194:216–22
- Roberts DJ, de Souza VC. A venue-based analysis of the reach of a targeted outreach service to deliver opportunistic community NHS Health Checks to “hard-to-reach” groups. Public Health. 2016 Aug;137:176–81.
- Atkins Lou, Stefanidou Chryssa, Chadborn Tim, Thompson Katherine, Michie Susan, Lorencatto Fabi. Influences on NHS Health Check behaviours: a systematic review. BMC public health. 2020;20(1):1359.
- Stuber J, Galea S, Link BG. Smoking and the emergence of a stigmatized social status. Soc Sci Med. 2008 Aug;67(3):420–30.
- Graham H. Smoking, Stigma and Social Class. Journal of Social Policy. 2012 Jan;41(1):83–99.
- Bidstrup Hugh, Brennan Leah, Kaufmann Leah, de la Piedad Garcia Xochitl. Internalised weight stigma as a mediator of the relationship between experienced/perceived weight stigma and biopsychosocial outcomes: a systematic review. International journal of obesity (2005). 2022;46(1):1–9.
- David Jean-Charles, Fonte David, Sutter-Dallay Anne-Laure, Auriacombe Marc, Serre Fuschia, Rascle Nicole, et al. The stigma of smoking among women: A systematic review. Social science & medicine (1982). 2024;340:116491.
- Banafshe Elahe, Javadifar Nahid, Abbaspoor Zahra, Karandish Majid, Ghanbari Saeed. Factors Influencing Weight Management in Pregnant Women with Overweight or Obesity: A Meta-Synthesis of Qualitative Studies. Journal of the Academy of Nutrition and Dietetics. 2024;124(8):964-994.e1.
- Auckburally Sameera, Davies Elena, Logue Jennifer. The Use of Effective Language and Communication in the Management of Obesity: the Challenge for Healthcare Professionals. Current obesity reports. 2021;10(3):274–81.
- Ricci-Cabello Ignacio, Ruiz-Pérez Isabel, Nevot-Cordero Adela, Rodríguez- Barranco Miguel, Sordo Luis, Gonçalves Daniela C. Health Care Interventions to Improve the Quality of Diabetes Care in African Americans: A systematic review and meta-analysis. Diabetes Care. 2013;36(3):760–8.
- Diabetes UK [Internet]. [cited 2024 Aug 27]. What is HbA1c?
Available from: https://www.diabetes.org.uk/guide-to-diabetes/managing-%20your-diabetes/hba1c - Nam Soohyun, Janson Susan, Stotts Nancy A, Chesla Catherine A, Kroon Lisa. Effect of Culturally Tailored Diabetes Education in Ethnic Minorities With Type 2 Diabetes. 2011
Available from: https://%20pubmed.ncbi.nlm.nih.gov/21747287/ - Singh Hardeep, Fulton Joseph, Mirzazada Sofia, Saragosa Marianne, Uleryk Elizabeth M, Nelson Michelle L. A. Community-Based Culturally Tailored Education Programs for Black Communities with Cardiovascular Disease, Diabetes, Hypertension, and Stroke: Systematic Review Findings. Journal of Racial and Ethnic Health Disparities. 2023;10(6):2986–3006.
- Wadi Noor M, Asantewa-Ampaduh Summor, Rivas Carol, Goff Louise M. Culturally tailored lifestyle interventions for the prevention and management of type 2 diabetes in adults of Black African ancestry: a systematic review of tailoring methods and their effectiveness. Public Health Nutrition. 2021;1–15.
- Goswami Aumeya, Poole Lydia, Thorlu-Bangura Zareen, Khan Nushrat, Hanif Wasim, Khunti Kamlesh, et al. The Use of Digital Health Interventions for Cardiometabolic Diseases Among South Asian and Black Minority Ethnic Groups: Realist Review. Journal Of Medical Internet Research. 2023;25:e40630–e40630.
- Smith Caroline E, Hill Sarah E, Amos Amanda. Impact of specialist and primary care stop smoking support on socioeconomic inequalities in cessation in the United Kingdom: a systematic review and national equity analysis. Addiction. 2020;115(1):34–46
- Desta Russom, Blumrosen Charlotte, Laferriere Heather E, Saluja Aades, Bruce Marino A, Elasy Tom A, et al. Interventions Incorporating Therapeutic Alliance to Improve Medication Adherence in Black Patients with Diabetes, Hypertension and Kidney Disease: A Systematic Review. Patient Preference And Adherence. 2022;Volume 16:3095–110.
- Hildebrand Janett A, Billimek John, Lee Jung-Ah, Sorkin Dara H, Olshansky Ellen F, Clancy Stephen L, et al. Effect of diabetes self-management education on glycemic control in Latino adults with type 2 diabetes: A systematic review and meta-analysis. Patient Education and Counseling. 2020;103(2):266–75.
- Padda Inderbir. Cardiovascular health amongst South Asian populations in British Columbia: A situational and comparative analysis of preventative strategies. Current problems in cardiology. 2024;49(6):102570.
- Amenyah Sophia D, Waters Diane, Tang Wen, Fenge Lee-Ann, Murphy Jane L. Systematic realist synthesis of health-related and lifestyle interventions designed to decrease overweight, obesity and unemployment in adults. BMC public health. 2022;22(1):2100.
- Herbozo Sylvia, Brown Kristal Lyn, Burke Natasha L, LaRose Jessica Gokee. A Call to Reconceptualize Obesity Treatment in Service of Health Equity: Review of Evidence and Future Directions. Current obesity reports. 2023;12(1):24–35.
- Bland Vanessa, Sharma Manoj. Physical activity interventions in African American women: A systematic review. Health Promotion Perspectives. 2017;7(2):52–9.
- Balk E M, Earley A, Raman G, Avendano E A, Pittas A G, Remington P L. Combined Diet and Physical Activity Promotion Programs to Prevent Type 2 Diabetes Among Persons at Increased Risk: A Systematic Review for the Community Preventive Services Task Force. Annals of Internal Medicine. 2015;163(6):437-+.
- Lei Fang, Zheng Ying. Smoking Cessation Interventions for Chinese American Smokers: A Systematic Review and Meta-Analysis. Asian Pacific Journal Of Cancer Prevention. 2023;24(3):753–68.
- Garg Rachel, McQueen Amy, Evbuoma-Fike Ebuwa I, Kreuter Matthew W. Re-examining phone counseling for smoking cessation: Does the evidence apply to low-SES smokers?. Patient education and counseling. 2022;105(7):1783–92.
- Connell Patricia, Wolfe Charles, McKevitt Christopher. Preventing stroke: a narrative review of community interventions for improving hypertension control in black adults. Health & Social Care In The Community. 2007;16(2):165–87.
- Kim MT, Han HR, Song HJ, Lee JE, Kim J, Ryu JP, et al. A Community- Based, Culturally Tailored Behavioral Intervention for Korean Americans With Type 2 Diabetes. Diabetes Educ. 2009 Nov 1;35(6):986–94.
- Pottie K, Hadi A, Chen J, Welch V, Hawthorne K. Realist review to understand the efficacy of culturally appropriate diabetes education programmes. Diabetic Medicine. 2013;30(9):1017–25.
- Onakomaiya Deborah, Cooper Claire, Barber Aigna, Roberts Timothy, Gyamfi Joyce, Zanowiak Jennifer, et al. Strategies to Improve Medication Adherence and Blood Pressure Among Racial/Ethnic Minority Populations: A Scoping Review of the Literature from 2017 to 2021. Current Hypertension Reports [Internet]. 2022
Available from: https://explore.openalex.org/works/W4296613395 - Rawal Lal, Sahle Berhe W, Smith Ben J, Kanda Kie, Owusu-Addo Ebenezer, Renzaho Andre M N. Lifestyle interventions for type 2 diabetes management among migrants and ethnic minorities living in industrialized countries: a systematic review and meta-analyses. BMJ Open Diabetes Research & Care. 2021;9(1):e001924.
- World Health Organization. Strengthening the performance of community health workers in primary health care: report of a WHO Study Group [meeting held in Geneva from 2 to 9 December 1987]. World Health Organization; 1989.
- Evans Joseph, White Patrick, Ha Howard. Evaluating the effectiveness of community health worker interventions on glycaemic control in type 2 diabetes: a systematic review and meta-analysis. Lancet (London, England). 2023;402 Suppl 1:S40.
- Bambra Clare L, Hillier Frances C, Cairns Joanne-Marie, Kasim Adetayo, Moore Helen J, Summerbell Carolyn D. How effective are interventions at reducing socioeconomic inequalities in obesity among children and adults? Two systematic reviews. Public Health Research. 2015;3(1):1–446.