What works: Funding models to address health inequalities

Mortality rates are higher in areas of greater deprivation, and life expectancy a decade shorter in the least affluent areas compared to most affluent areas in England. Addressing inequalities through funding is crucial given its impact on service provision, workforce distribution and consequently patient outcomes. This brief examines the evidence on how health care funding can be structured to reduce health and care inequalities.
What works: Funding models to address health inequalities[PDF 552kb]
Download documentSummary
Health inequalities have a profound effect on individual lives and lead to increased health care demand, higher costs, and a negative impact on the nation’s long-term economic prosperity. Beyond addressing social determinants of health, action on health care system design to reduce inequalities can significantly enhance overall system efficiency. Funding plays a crucial role as it directly influences the distribution of resources and incentives to deliver high quality care. Here, we examine evidence on how health care funding can be structured to reduce health and care inequalities.
Based on a review of 46 articles, we found that while there is a lack of robust studies because of the challenges of conducting research in this area, there are several evidence-based principles of how inequalities can be addressed through more equitable funding models. Key findings were:
- Capitation funding is associated with more equitable outcomes than fee-for-service.
- Pay-for-performance systems without equity considerations compound funding inequalities by directing more money to areas of lower clinical need.
- Adjusting funding, especially pay-for-performance, to account for socioeconomic or health differences, would improve efficiency of funding, reduce funding inequalities and likely reduce health and care inequalities.
- Payments for performance could also be improved by comparing performance between similar organisations, paying for improvements, reducing exception reporting, and rewarding organisations for improving health inequalities.
- Increased privatisation is associated with increased inequalities, but increased marketisation in a publicly funded system is not.
- Targeting funding to specific disadvantaged groups can improve health inequalities.
Current challenges
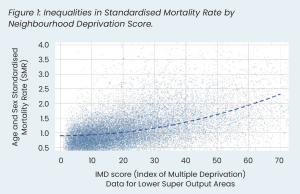
Inequalities in health are well documented internationally and are recognised as an important issue for policymakers to tackle [1][2][3]. In England, mortality rates are higher in areas with greater deprivation (Figure 1) and life expectancy in the least affluent areas is a decade shorter than the most affluent areas [4][5]. The difference in healthy life expectancy is also significant; healthy life expectancy is 18 years higher in the most affluent areas compared with the least affluent areas [6].
It is not just morally, but also economically imperative to tackle health inequalities. Prior to COVID, health inequalities’ annual costs were estimated as £4.8 billion to the NHS, £31 billion in lost productivity, and between £20–32 billion in lost tax and increased benefit payments [7]. This is likely to have risen after the pandemic.
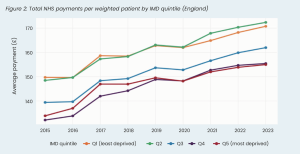
Addressing health inequalities requires policy interventions to address key determining factors for health targeting underlying social inequalities [1][8][9]. However, action must also address inequalities across health care systems. Addressing inequalities in funding is imperative given its impact on service provision, workforce and subsequently patient outcomes [10][11][12]. In addition to designing funding to improve inequalities, it is vital that existing funding models do not compound them. For example, general practices in more affluent areas receive more funding per patient compared to less affluent areas when weighting for clinical need [2]. That the least affluent areas have the worst health, yet receive relatively less funding, highlights the persistence of the Inverse Care Law: those who most need high-quality health care have the least access to it [13].
There are three common funding models described in the literature: capitation, fee-for-service (FFS) and pay-for-performance (P4P). In England, general practice is predominantly funded through capitation with P4P and FFS funding schemes providing additional incentives. Meanwhile, FFS models dominate funding of acute hospitals.
To prevent funding structures from worsening health inequalities, it is crucial, at the very least, to align funding with clinical need. More ambitiously, reversing both funding inequalities and the Inverse Care Law would require allocating even more resources to areas with the highest need, beyond what their clinical demands might suggest. This can be accomplished by introducing new funding models or modifying existing ones. The NHS uses several different funding models and here we review the evidence of the types of funding models that are most likely to address health inequalities.
Summary of evidence
We identified studies from: 1) A living evidence map from the Health Equity Evidence Centre [14]; 2) a search of electronic databases (MEDLINE, EMBASE, Cochrane); and 3) snowballing references. In total we screened 4328 articles and prioritised 46 articles for review. Latest reviews with the greatest relevance to the UK context were prioritised in reporting.
This review identifies a range of evidence regarding how health care funding can be used to address health inequalities, and what funding models result in increased or decreased inequalities. There is a lack of randomised, well-controlled research that examines how funding models affect health inequalities. This is largely due to methodological challenges common to a lot of public policy research. For example, it can be hard to isolate the impact of funding changes without a clear point of comparison, and randomisation of interventions rarely occurs.
Despite this, existing research studies provide some clear guidance about which types of funding models are more or less likely to address health inequalities. We divide the evidence into four categories:
- Impact of capitation, fee-for-service, and pay-for-performance on health inequalities
- Adjusting existing funding models to reduce health inequalities
- Direct funding to organisations serving specific disadvantaged groups
- Impact of increased privatisation and marketisation
1. Impact of capitation, fee-for-service and pay-for-performance on health inequalities
Capitation and fee-for-service
There was limited relevant evidence found regarding the introduction of capitation and FFS models on inequalities. The limited evidence suggests that capitation payments are more likely to address health inequalities compared to FFS. Tao and colleagues (2016) reviewed six studies that explored health inequalities of patients in capitation-based plans compared to FFS [15]. Two US studies and one Canadian study in the review found that organisations with capitation plans were associated with lower inequalities by ethnicity in access to care. Both US studies also reported reduced inequalities in continuity of care and quality of care in organisations with capitation plans. In contrast, two studies reported that there was generally little difference in inequalities between plans. This is not to say that all capitation models are necessarily equitable, or that they can’t be made more equitable. For example, the Carr-Hill formula, which calculates capitation payments to general practices in England, has been criticised for not considering socioeconomic variables such as deprivation indices [5][16][17].
Pay-for-performance
Over-reliance on P4P schemes that reward quality alone can exacerbate inequalities in funding. Studies identified a “reverse Robin Hood effect”, where GP practices with relatively healthy patients, mostly in affluent areas, receive more funding [18][19]. We know from both UK and international literature that health care organisations that serve socioeconomically disadvantaged and ethnically diverse groups tend to have worse quality of care and therefore are likely to receive less funding in P4P programmes. Markovitz and colleagues (2017) reviewed 58 studies from the UK, US and Canada and found that worse performance was associated with practices and hospitals that served poorer patients and more patients from racial and ethnic minorities, but not by any other patient factors, including insurance type, gender, age, or patient health [20][21].
Direct evidence of the impact of P4P schemes on health and care inequalities is limited [22][23]. In England, the Quality and Outcomes Framework (QOF) is the largest P4P programme. When introduced, there was an initial widening in the quality of care between more and less affluent areas, followed by a narrowing [24][25][26]. The QOF also narrowed inequalities by age [25][26][27] and widened inequalities by sex in favour of male patients [24][26][27][28]. Ethnicity showed no clear overall pattern [15][24][25][26][27]. Importantly, this evidence is observational, and the effects of the QOF cannot be distinguished from other co-occurring factors such as a cross-government Health Inequalities Strategy, which was associated with reduced socioeconomic health inequalities [9][29][30]. There is limited evidence on the long-term effects of the QOF on inequalities. Furthermore, research has suggested that the QOF does not significantly reduce mortality related to heart disease, cancer or other conditions [31].
Beyond the QOF, there is limited evidence on the impact of P4P on inequalities. For example, Eijkenaar and colleagues (2013) examined P4P and found that P4P led to a narrowing of inequalities, but the study relied on four early studies of the QOF [32]. Similarly, other reviews were highly reliant on the QOF for outcomes, limiting the impact of conclusions due to the observational nature of studies, and lack of similarity to other P4P schemes [24][33][34]. A Cochrane review [22] identified only one study assessing the impact of P4P in an inpatient setting. This US study found that financially awarding or penalising hospitals for quality was associated with increased inequalities in access between ethnic groups. A systematic review of value-based health care schemes in the US found inconclusive evidence, given large heterogenicity of studies [23].
2. Adjusting existing funding models to reduce health inequalities
Adjusting capitation
Capitation models can be adjusted to account for measures of socioeconomic status. Such an approach is used internationally [35], but not in the UK [5][16][17]. Doing so would improve funding; a recent study found that adjusting the Carr-Hill formula in England by deprivation data would not just improve funding equity, it would significantly enhance funding efficiency. This study also found that adjusting total general practice funding would have significant effects, with an even larger improvement in efficiency [5].
Adjusting pay-for-performance
Conway and colleagues (2022) examined how P4P programmes can be optimised to reduce inequalities [19]. Two key adjustments were supported by quantitative evidence. First, good quality, consistent evidence was found for adjusting either performance or payments for the difficulty of achieving the target [36][37][38]. For example, this could involve adjusting for health factors, such as comorbidities or socioeconomic factors to ensure that practices are paid relative to the difficulty of meeting the payment threshold [28]. One criticism of this approach is that if results are adjusted, and only adjusted results published, this may conceal socioeconomic differences in health, as the underlying differences would be hidden [19]. This highlights the importance of reporting both unadjusted and adjusted statistics and payments. Second, financial incentives could be reimbursed according to performance against health care organisations grouped by socioeconomic or clinical factors. Wholey and colleagues (2018) examined the best ways to compare quality of care across health care organisations in Minnesota. The authors found that grouping practices by socioeconomic factors was a more accurate way of explaining variations in performance than simply adjusting for these [39].
Two further initiatives to reduce inequalities through P4P are described in the literature but were primarily based on expert opinion rather than quantitative evidence. First, designing metrics to either target inequalities directly, or indirectly at specific populations, conditions, processes and outcomes, would be expected to improve inequalities [19]. Second, improvement from baseline measures rather than absolute quality was suggested to be more equitable [19][28].
Exclusion of patients from P4P schemes, especially in the QOF, was noted to be of significant concern for inequalities. For example, exception reporting within the QOF permits practices to exclude certain patients from target calculations based on patient compliance, disease status, medication suitability, availability of services or patients being new to the practice. This can exclude underserved groups with unintended consequences: patients who are older, less affluent, and experience multiple long-term conditions who are exception-reported patients are more likely to die in the following year [25][28][40].
Adjusting local health and care budgets
There is good evidence that adjusting existing funding to local health and care systems reduces inequalities. Barr and colleagues (2014) published an analysis of changes to the NHS allocation formula in 2002 that resulted in more funding being allocated to socioeconomically disadvantaged areas. They found significant reductions in mortality inequalities and overall improvements in mortality nationally, which were driven by improvements in areas with higher levels of deprivation: each additional £10m of resources in the least affluent areas was associated with a reduction of 4 deaths per 100,000 in males and 1.8 deaths per 100,000 in females. This association was not significant in the most affluent areas [41]. An example of this in action at a local level is shown below.
3. Direct funding to organisations serving specific disadvantaged groups
Providing unconditional cash transfers to organisations that service certain disadvantaged populations can reduce health inequalities. Evidence of this comes from transfers targeting homeless people [42], indigenous populations [43] and rural communities [44][45]. Gibson and colleagues (2015) reviewed 13 studies and found evidence that increasing funding specifically targeted at minority groups, with poorer health, was effective in narrowing inequalities [43]. Three studies included in the review examined indigenous groups in the US, Australia and New Zealand who had worse type 2 diabetes outcomes compared to the national average. Of the two studies that were successful in improving health outcomes, both involved the unconditional transfer of financial resources to facilitate improved care. The third used a fee-for-service model, where providers were paid per diabetic care plan, and failed to show a narrowing in inequalities.
4. Impact of increased role of the private sector and marketisation
Countries with more publicly funded health and care services tend to have lower inequalities. A review of European healthcare funding identified that increased private ownership of healthcare services is associated with increased socioeconomic inequalities in access [46]. This review also identified two studies that found that increases in user fees and out of pocket payments resulted in increased health inequalities.
Increasing health care delivery through higher use of privately owned, for-profit organisations can increase inequalities. Burstrom and colleagues (2017) explored Swedish health reform between 2008 and 2010 which encouraged privately funded primary health care practices to the market and promoted patients to choose between them [47]. Overall, this was associated with increased inequalities. Private practices were less likely to be found in areas with populations with worse health. Additionally, while access increased for all groups it did so less for those with worse health. Reforms acted as a barrier to integrated care for those with worse health. A recent study found that areas with a higher increase in private provision saw a decrease in avoidable hospitalisations, but an increase in socioeconomic inequalities in hospitalisation rates [48].
Evidence from the UK suggests that procompetitive reforms, within a predominantly nationalised service, are less strongly associated with increased inequalities than privatisation. These procompetitive reforms throughout the 2000s in the UK include 1) increased independent sector hospital access to the NHS funded market, 2) increased patient choice of care location and 3) introduction of a fixed price system of payment [49]. While there was much commentary and theoretical evidence suggesting that this could widen inequalities [50], such a change was not seen [49][51][52]. Cookson and colleagues (2013) found that increased competition among hospitals in the UK led to more care in socioeconomically disadvantaged areas and a decrease in inequalities [52]. This difference in findings is likely attributable to competition being small and most hospital services continued to be supplied by public hospitals who did not have strong incentives to select healthier patients – a process known as “cream skimming” [49].
Limitations
The search strategy for this evidence brief covers existing international review articles identified through the HEEC evidence maps, a search on three databases, and snowball searching. While such an approach is sufficiently rigorous to capture a wide range of evidence, some primary studies that are not found in the identified reviews could have contributed further to this brief. As is common for research around health care funding, much of the evidence was observational rather than controlled, randomised or experimental.
What works: key recommendations
| Recommendation | Target audience | GRADE certainty |
| Local and national decision makers should ensure that funding models allocate resources proportionate to need. | NHS England, DHSC, ICBs and local authorities | ⊕ ⊕ ⊕ ⊕
High |
| Health inequalities should be considered in funding decisions to ensure a more efficient distribution of funding relative to clinical need. | NHS England, DHSC, ICBs and local authorities | ⊕ ⊕ ⊕
Moderate |
| Increasing funding through equitable capitation models is likely to address inequalities compared to fee-for-service approaches. | NHS England, DHSC and ICBs | ⊕ ⊕
Low |
| Pay-for-performance reimbursement models without any equity adjustment are likely to result in more funding to areas with better health, exacerbating inequalities. | NHS England, DHSC and ICBs | ⊕ ⊕ ⊕
Moderate |
| Funding, especially through pay-for-performance reimbursement, should be weighted to account for clinical need, including accounting for socioeconomic disadvantage. | NHS England, DHSC and ICBs | ⊕ ⊕ ⊕
Moderate |
| Pay-for-performance should reward health care organisations for reducing inequalities or achieving high performance in outcomes that would likely lead to a reduction in inequalities. | NHS England, DHSC and ICBs | ⊕
Very low |
| Organisations in more affluent areas tend to be able to respond quicker to policy change, therefore practices in more disadvantaged areas should be provided with more implementation support to achieve the policy objectives. | NHS England, DHSC and ICBs | ⊕ ⊕
Low |
| Exception reporting, for example in the QOF, should be reviewed to ensure that it does not increase inequalities, such as reducing time that patients can be excluded after joining the list, or removing the criteria that patients can be exception reported if not engaging with three postal letters. | NHS England, DHSC and ICBs | ⊕ ⊕ ⊕
Moderate |
| Any policy which increases the role of the private sector should be treated with caution and mitigations introduced to ensure that it does not increase inequalities. | NHS England, DHSC and ICBs | ⊕ ⊕ ⊕
Moderate |
| Funding through unconditional cash transfers to organisations serving specific disadvantaged communities that experience poor health and care should be considered. | NHS England, DHSC, ICBs and local authorities | ⊕ ⊕ ⊕
Moderate |
*GRADE certainty communicates the strength of evidence for each recommendation.
Recommendations which are supported by large trials will be graded highest whereas those arising from small studies or transferable evidence will be graded lower. The grading should not be interpreted as priority for policy implementation – i.e. some recommendations may have a low GRADE rating but likely to make a substantial difference.
How this brief was produced
What is the Living Evidence Map on what works to achieve equitable lipid management in primary care?
Using AI-powered software called EPPI-Reviewer, the Health Equity Evidence Centre has developed a Living Evidence Map of what works to address health inequalities in primary care. The software identifies research articles that examine interventions to address inequalities. The evidence map contains systematic reviews, umbrella reviews. More information can be found on the Health Equity Evidence Centre website.
Funding
This Evidence Brief has been commissioned by NHS England to support their statutory responsibilities to deliver equitable health care. Policy interventions beyond health care services were not in scope. The content of this brief was produced independently by the authors and do not necessarily reflect the views of NHS England.
Suggested citation
Holdroyd I, Dehn Lunn A, Harasgama S, Painter H, Pearce H, Torabi P, Vodden A, Wong YL, Ford J. Evidence brief: What works: Funding models to address health inequalities. Health Equity Evidence Centre; 2024
References
- Marmot M. Health equity in England: the Marmot review 10 years on. The Health Foundation. 2020.
- LaVeist TA, Perez-Stable EJ, Richard P, Anderson A, Isaac LA, Santiago R, et al. The Economic Burden of Racial, Ethnic, and Educational Health Inequities in the US. JAMA. 2023;329(19):1682- 92.
- Karanikolos M, Kentikelenis A. Health inequalities after austerity in Greece. Int J Equity Health. 2016;15:83.
- Office for National Statistics. Mortality statistics in England and Wales QMI 2022
Available from: https://%20www.ons.gov.uk/peoplepopulationandcommunity/%20birthsdeathsandmarriages/deaths/methodologies/%20mortalitystatisticsinenglandandwalesqmi. - Holdroyd I, Appel C, Massou E, Ford J. Adjusting primary-care funding by deprivation: a cross-sectional study of lower-superoutput- areas in England. BJGP Open. 2024.
- The Kings Fund. Health inequalities in a nutshell 2024
Available from: https://www.kingsfund.org.uk/insight-and-analysis/dataand-%20charts/health-inequalities-nutshell#:~:text=People%20%20living%20in%20the%20most,and%2086%20years%20in%20%20Kensington - Public Health England. Inclusive and sustainable economies: leaving no one behind 2021
- Marmot M, Allen J, Goldblatt P, Boyce T, McNeish Dea. Fair Society, Healthy Lives – The Marmot Review: Strategic review of health inequalities in England post-2010. 2010.
- Vodden A, Holdroyd I, Bentley C, Marshall L, Barr B, Massou E, et al. Evaluation of the national governmental efforts between 1997 and 2010 in reducing health inequalities in England. Public Health. 2023;218:128-35.
- Salant N, Massou E, Awan H, Ford JA. Does workforce explain the relationship between funding and patient experience? A mediation analysis of primary care data in England. BMJ Open. 2024;14(2):e072498.
- L’Esperance V, Sutton M, Schofield P, Round T, Malik U, White P, et al. Impact of primary care funding on secondary care utilisation and patient outcomes: a retrospective cross-sectional study of English general practice. Br J Gen Pract. 2017;67(664):e792-e9.
- McLean G, Guthrie B, Mercer SW, Watt GC. General practice funding underpins the persistence of the inverse care law: crosssectional study in Scotland. Br J Gen Pract. 2015;65(641):e799- 805.
- Hart JT. The inverse care law. Lancet. 1971;1(7696):405-12.
- Health Equity Evidence Centre. Health Equity Evidence Centre 2024
Available from: https://www.heec.co.uk - Tao W, Agerholm J, Burström B. The impact of reimbursement systems on equity in access and quality of primary care: A systematic literature review. BMC Health Serv Res. 2016;16(1):542.
- Kontopantelis E, Mamas MA, van Marwijk H, Ryan AM, Bower P, Guthrie B, et al. Chronic morbidity, deprivation and primary medical care spending in England in 2015-16: a cross-sectional spatial analysis. BMC Medicine. 2018;16(1):19.
- Levene LS, Baker R, Bankart J, Walker N, Wilson A. Socioeconomic deprivation scores as predictors of variations in NHS practice payments: a longitudinal study of English general practices 2013- 2017. Br J Gen Pract. 2019;69(685):e546-e54.
- Mann O, Bracegirdle T, Shantikumar S. The relationship between Quality and Outcomes Framework scores and socioeconomic deprivation: a longitudinal study. BJGP Open. 2023;7(4):BJGPO.2023.0024.
- Conway A, Satin D. The role of pay-for-performance in reducing healthcare disparities: A narrative literature review. Prev Med. 2022;164:107274.
- Markovitz AA, Ryan AM. Pay-for-Performance: Disappointing Results or Masked Heterogeneity? Med Care Res Rev. 2017;74(1):3- 78.
- Shakir M, Armstrong K, Wasfy JH. Could Pay-for-Performance Worsen Health Disparities? J Gen Intern Med. 2018;33(4):567-9.
- Mathes T, Pieper D, Morche J, Polus S, Jaschinski T, Eikermann M. Pay for performance for hospitals. Cochrane Database of Systematic Reviews. 2019(7).
- Kim H, Mahmood A, Hammarlund NE, Chang CF. Hospital valuebased payment programs and disparity in the United States: A review of current evidence and future perspectives. Front Public Health. 2022;10:882715.
- Alshamsan R, Millett C, Majeed A, Khunti K. Has pay for performance improved the management of diabetes in the United Kingdom? Primary care diabetes. 2010;4(2):73-8.
- Annemans L, Boeckxstaens P, Borgermans L, De Smedt D, Duchesnes C, Heyrman J, et al. Advantages, disadvantages and feasibility of Pay-for-Quality programs in Belgium. BMC Health Services Research. 2009;10(2):A6.
- Boeckxstaens P, Smedt DD, Maeseneer JD, Annemans L, Willems S. The equity dimension in evaluations of the quality and outcomes framework: a systematic review. BMC health services research. 2011;11:209.
- Steel N, Willems S. Research learning from the UK Quality and Outcomes Framework: a review of existing research. Quality in primary care. 2010;18(2):117-25.
- Gillam SJ, Siriwardena AN, Steel N. Pay-for-performance in the United Kingdom: impact of the quality and outcomes framework: a systematic review. Annals of family medicine. 2012;10(5):461-8.
- Barr B, Higgerson J, Whitehead M. Investigating the impact of the English health inequalities strategy: time trend analysis. BMJ. 2017;358:j3310.
- Holdroyd I, Vodden A, Srinivasan A, Kuhn I, Bambra C, Ford JA. Systematic review of the effectiveness of the health inequalities strategy in England between 1999 and 2010. BMJ Open. 2022;12(9):e063137.
- Ryan AM, Krinsky S, Kontopantelis E, Doran T. Long-term evidence for the effect of pay-for-performance in primary care on mortality in the UK: a population study. The Lancet. 2016;388(10041):268-74.
- Eijkenaar F, Emmert M, Scheppach M, Schöffski O. Effects of pay for performance in health care: a systematic review of systematic reviews. Health Policy. 2013;110(2-3):115-30.
- Van Herck P, De Smedt D, Annemans L, Remmen R, Rosenthal MB, Sermeus W. Systematic review: Effects, design choices, and context of pay-for-performance in health care. BMC health services research. 2010;10:247.
- Wagenschieber E, Blunck D. Impact of reimbursement systems on patient care – a systematic review of systematic reviews. Health Econ Rev. 2024;14(1):22.
- Penno E, Gauld R, Audas R. How are population-based funding formulae for healthcare composed? A comparative analysis of seven models. BMC Health Services Research. 2013;13(1):470.
- Damberg CL, Elliott MN, Ewing BA. Pay-For-Performance Schemes That Use Patient And Provider Categories Would Reduce Payment Disparities. Health Affairs. 2015;34(1):134-42.
- Glance LG, Kellermann AL, Osler TM, Li Y, Li W, Dick AW. Impact of Risk Adjustment for Socioeconomic Status on Risk-adjusted Surgical Readmission Rates. Ann Surg. 2016;263(4):698-704.
- Gonzalez AA, Motaganahalli A, Saunders J, Dev S, Dev S, Ghaferi AA. Including socioeconomic status reduces readmission penalties to safety-net hospitals. J Vasc Surg. 2024;79(3):685-93. e1.
- Wholey DR, Finch M, Kreiger R, Reeves D. Public Reporting of Primary Care Clinic Quality: Accounting for Sociodemographic Factors in Risk Adjustment and Performance Comparison. Population Health Management. 2018;21(5):378-86.
- Forbes L, Marchand C, Peckham S. Review of the Quality and Outcomes Framework in England. 2016.
- Barr B, Bambra C, Whitehead M. The impact of NHS resource allocation policy on health inequalities in England 2001-11: longitudinal ecological study. BMJ. 2014;348:g3231.
- White BM, Newman SD. Access to primary care services among the homeless: a synthesis of the literature using the equity of access to medical care framework. J Prim Care Community Health. 2015;6(2):77-87.
- Gibson OR, Segal L. Limited evidence to assess the impact of primary health care system or service level attributes on health outcomes of Indigenous people with type 2 diabetes: a systematic review. BMC health services research. 2015;15:154.
- Gizaw Z, Astale T, Kassie GM. What improves access to primary healthcare services in rural communities? A systematic review. BMC Prim Care. 2022;23(1):313.
- Sempowski IP. Effectiveness of financial incentives in exchange for rural and underserviced area return-of-service commitments: systematic review of the literature. Can J Rural Med. 2004;9(2):82- 8.
- Gelormino E, Bambra C, Spadea T, Bellini S, Costa G. The Effects of Health Care Reforms on Health Inequalities: A Review and Analysis of the European Evidence Base. International Journal of Health Services. 2011;41(2):209-30.
- Burstrom B, Burstrom K, Nilsson G, Tomson G, Whitehead M, Winblad U. Equity aspects of the Primary Health Care Choice Reform in Sweden – a scoping review. International journal for equity in health. 2017;16(1):29.
- Gustafsson PE, Fonseca-Rodríguez O, San Sebastián M, Burström B, Mosquera PA. Evaluating the impact of the 2010 Swedish choice reform in primary health care on avoidable hospitalization and socioeconomic inequities: an interrupted time series analysis using register data. BMC Health Services Research. 2024;24(1):972.
- Cookson R, Laudicella M, Li Donni P, Dusheiko M. Effects of the Blair/ Brown NHS reforms on socioeconomic equity in health care. J Health Serv Res Policy. 2012;17 Suppl 1:55-63.
- Fotaki M, Roland M, Boyd A, McDonald R, Scheaff R, Smith L. What benefits will choice bring to patients? Literature review and assessment of implications. J Health Serv Res Policy. 2008;13(3):178-84.
- Cooper ZN, McGuire A, Jones S, Le Grand J. Equity, waiting times, and NHS reforms: retrospective study. Bmj. 2009;339:b3264.
- Cookson R, Laudicella M, Donni PL. Does hospital competition harm equity? Evidence from the English National Health Service. Journal of Health Economics. 2013;32(2):410-22.