The EQUALISE study, funded by NIHR and led by the University of Cambridge, explored what types of interventions in general practice increase or decrease inequalities among people with, or at risk of, cardiovascular disease, cancer, diabetes and/or chronic obstructive pulmonary disease. A realist review was carried out to identify for whom these interventions and aspects of care work best, why, and in what circumstances.
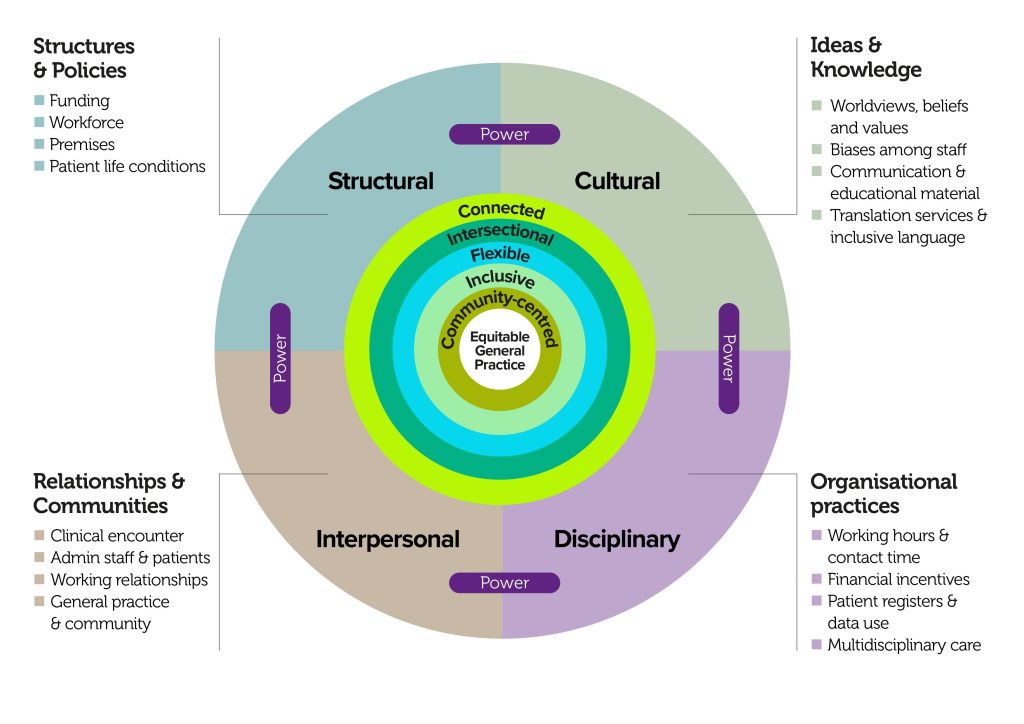
We identified five guiding principles for designing equitable primary care:
- Connected: Interventions and services should be understood, designed, and delivered as connected components of coordinated action against health inequalities.
- Intersectional: Care should adopt an intersectional perspective to account for the different impact of services and interventions among patients according to their circumstances and experience of (multiple) disadvantage.
- Flexible: Care delivery should be flexible enough to make allowances for different patient needs and preferences in terms of time, accessible communication, location, and provided support.
- Inclusive: We need to cultivate an organisational culture that is less western-centric and normative to ensure that people are not excluded due to wrong assumptions about who they are, what they need, and how they ‘should’ behave.
- Community-centred: Everybody involved in care should have a say in how it is conceived, (re)designed, and delivered including clinical and non-clinical members of staff, patients, and their networks.
These guiding principles cut across four action areas: structural, cultural, interpersonal and disciplinary.
At the heart of these principles is the acknowledgement that understanding and addressing the unequal distribution of power is fundamental.