Harnessing Health Impact Assessments for a fairer and healthier future

A healthy population is key to citizen wellbeing, a productive economy and manageable public services. Policy decisions on jobs, income, housing, education, transport and green space have a major impact on health, but do not involve the Department of Health and Social Care. As the government sets out policies to deliver on its manifesto commitments, how can we ensure health is considered across government, mitigating the potential adverse impacts, ensuring equity and accentuating the positives? Here we argue that Health Impact Assessments are a key tool to cross-government action on health and health inequalities.
The new government aims to “tackle the social determinants of health, halving the gap in healthy life expectancy between the richest and poorest regions in England”. The ambition and boldness are welcome. It will require action across all government departments, not just the Department of Health and Social Care (DHSC), because we know the key drivers of health go beyond the NHS and include income, housing, employment, education and access to green space.
Health Impact Assessment (HIA) is a tool that helps policymakers across government, particularly in non-health departments, consider the implications of their decisions on health and health inequalities. Here we share a project commissioned by the Health Foundation to explore the use of HIAs across government through a literature review, expert discussions, Freedom of Information requests and comparing international practice.
What is a Health Impact Assessment?
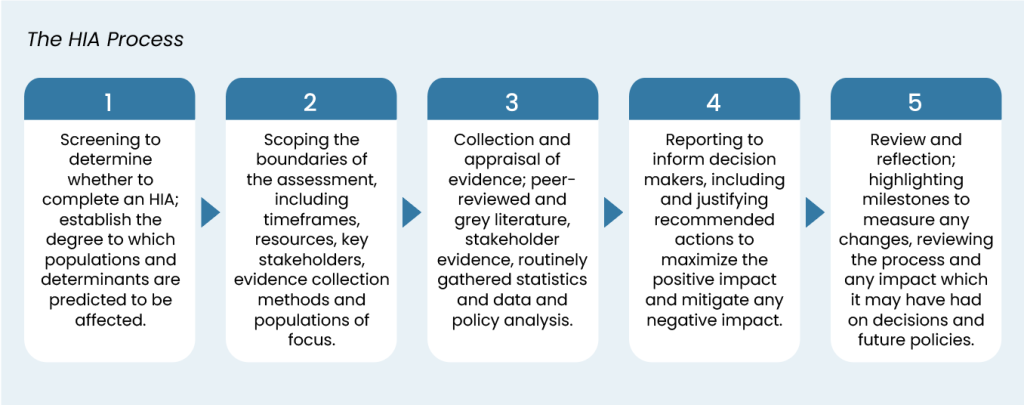
The HIA process varies from organisation to organisation, but there are a few common components. These include deciding if an HIA is necessary and proportionate, setting boundaries, collecting data on potential health and inequalities impacts, making recommendations and reviewing the assessment.
Are Health Impact Assessments needed?
New ministers are currently setting out a raft of health and non-health policies. Most of them will have some impact on health and health inequalities, directly or indirectly. For example, the government’s “Green Prosperity Plan” aims to create 650,000 jobs by 2030 through investments in green infrastructure and technologies. HIAs are needed to help policy makers consider the likely impact on health and health inequalities to build in mitigations and amplify positive benefits. For example, this may include the location of investment to provide high quality jobs, skills development pathways, educational investment and pressure on GP surgeries and hospitals.
Without an HIA, there is a risk that one part of government is setting out a health agenda while at the same time another department is implementing policies with an adverse impact on health and health inequalities.
There are good examples of HIAs leading to a change in policy direction, such as the example of shale oil and gas and coal bed methane in Scotland.
HIA Case Study: Potential consequences of shale oil and gas, and coal bed methane in Scotland
A national-scale HIA was conducted to investigate the potential consequences of developing shale oil and gas, and coal bed methane to Scotland, known as unconventional oil and gas (UOG). At the time of its completion, this was the first HIA to comprehensively evaluate the health effects of UOG, including fracking. This HIA was undertaken at the requested of the Scottish Government to inform a decision about whether to maintain a moratorium on UOG in Scotland.
The HIA included a systematic review of scientific research on UOG hazards, exposures and health impacts, and stakeholder workshops with community groups, industry and public sector agencies. The HIA identified that UOG was likely to increase several airborne and waterborne hazards and increase risk of seismic activity, although there was insufficient evidence of the physical health impacts of these exposures. It also found sufficient evidence that levels of airborne silica were likely to occur at levels that could pose a risk to the health of nearby residents and UOG workers. It identified qualitative evidence of UOG impacts on wider determinants of health, including traffic-related impacts, housing availability, environmental degradation, loss of community identity, control and social capital; increased demands on local services; inequalities in the distribution of impacts especially on those with existing poor health.
Positive impacts were also identified including economic benefits, provision of training and jobs, investment in and improvement of local infrastructure and services. The HIA was considered alongside other assessments and a public consultation to inform the Scottish Government decision not to proceed with UOG in Scotland. This HIA has been recognised as an approach that can be employed internationally to inform policymakers in assessing UOG proposals.
What are we proposing?
HIAs are not a silver bullet. Implemented poorly and they become a bureaucratic burden and perceived as a tick box exercise. However, implemented well, with a focus on improving decision making rather than completing a form, they can be a catalyst for organisational change and cross-government action on health and health inequalities.
Based on our review we propose:
- Mandatory Implementation: If HIAs remain voluntary, their use will remain ad hoc. HIAs should be a compulsory part of the decision-making process for all significant policy changes across government departments.
- Dedicated Resources and Support Infrastructure: HIAs need dedicated resources and skills. We believe an HIA unit is needed to provide the necessary resources, training, and guidance. Relying on individual government departments to resource HIAs is likely to lead to poor-quality and ineffective HIAs.
- Long-term Commitment: HIAs are a tool for better decision-making and long-term organisational change. They take time to embed. Securing long-term funding and support for HIAs is needed, ensuring that they are not vulnerable to changes in government or budget cuts.
- Continuous Improvement and Monitoring: We need agreed guidelines for conducting and monitoring HIAs, and to consider how we expand community engagement and advanced methodologies like machine learning. Some of this guidance already exists and simply needs to be enacted.
The impact of these measures will be most evident in the long term, as they contribute to a gradual but significant change in organisational culture, promoting transparency and a sustained focus on health equity.
Example of HIAs in action: Wales HIA Support Unit
The Public Health Wales Act 2017 places a duty on Welsh Ministers to carry out HIAs under specified circumstances. Furthermore, the Wellbeing of Future Generations Act (WFGA) 2015, while not explicitly mandating HIA, requires public bodies to address health inequalities when considering any policies, promoting the Health In All Policy approach and facilitating an environment for HIA uptake. Progress in Wales is attributed to both enabling legislation and the presence of dedicated long-term support from the Wales HIA Support Unit (WHIASU).
In addition to carrying out HIAs, WHIASU provides expert knowledge, practically experienced advice, resources, training and guidance. Subsequent policy making, and ongoing financial and political commitment from the Welsh Government has strengthened the implementation of HIA throughout Wales. Supplementary to this is Quality Assurance Review Framework for HIA, a framework to support and guide quality assurance review of HIA which aims to provide guidance for both commissioners and reviewers of HIA.
You can find out more about WHIASU here https://phwwhocc.co.uk/whiasu/
Funding: Health Foundation
Project team: Heidi Lynch, Ian Holdroyd, Martin Birley, Daniel Black, Ben Cave, Margaret Douglas, Rowena Ekermawi, Liz Green, Fiona Haigh, Ben Harris-Roxas, Monica O’Mullane, Joanna Purdy, Anna Stevenson, Salim Vohra, John Ford
Read our evidence brief here

Making Health in All Policies a reality: A call for Health Impact Assessments across government to improve health and address health inequalities
In this evidence brief, we examine the current state of Health Impact Assessments (HIAs) in the UK and their potential to reduce health inequalities. HIAs are essential to the Health in All Policies approach, which integrates health considerations across government. We offer recommendations to increase HIA use, emphasising the need for stronger leadership and dedicated resources to fully embed HIAs in national policy-making.