Making Health in All Policies a reality: A call for Health Impact Assessments across government to improve health and address health inequalities

In this evidence brief, we examine the current state of Health Impact Assessments (HIAs) in the UK and their potential to reduce health inequalities. HIAs are essential to the Health in All Policies approach, which integrates health considerations across government. We offer recommendations to increase HIA use, emphasising the need for stronger leadership and dedicated resources to fully embed HIAs in national policy-making.
Evidence brief – making health in all policies a reality[PDF 344kb]
Download documentSummary
Unequal distribution of the wider determinants of health across the social gradient creates and exacerbates health inequalities. Many of these factors are outside the direct control of the Department of Health and Social Care (DHSC). Embedding a national government approach for health improvement is challenging.
A Health in All Policies (HiAP) approach describes how health and health equity can be improved through embedding consideration of health in cross-government decision making. Health Impact Assessments (HIAs) are a mechanism for delivering an HiAP approach across national and local governments, creating the conditions for healthy lives. Despite advocacy from health-experts and progressive international examples, HIA activity in England is currently sporadic. Stronger leadership and dedicated resources are required to embed HIAs in national government and optimise their utility.
Why do we need to consider Health in All Policies?
Growth in life expectancy in the UK, along with many other high-income countries, has stalled since about 2010 with latest figures showing a drop in the 2018-2020 period compared with 2015-2017 [1]. The number of working age people reporting a long-term condition has increased by 6% over the past 10 years (from 29% to 35%) [2]. Since the pandemic, the number of people of working age who cannot work because of ill health has risen by around 400,000 [2]. The most deprived population groups live shorter lives with more years spent in ill health [3]. Inequalities in health are driven by inequalities in the wider determinants of health; including socioeconomic status, housing, transport, access to healthcare, social circumstances and environmental stressors.
Many of these determinants are outside the direct control of the Department of Health and Social Care. Health in All Policies (HiAP) is an approach to embedding health considerations across local and national government.
What are Health Impact Assessments?
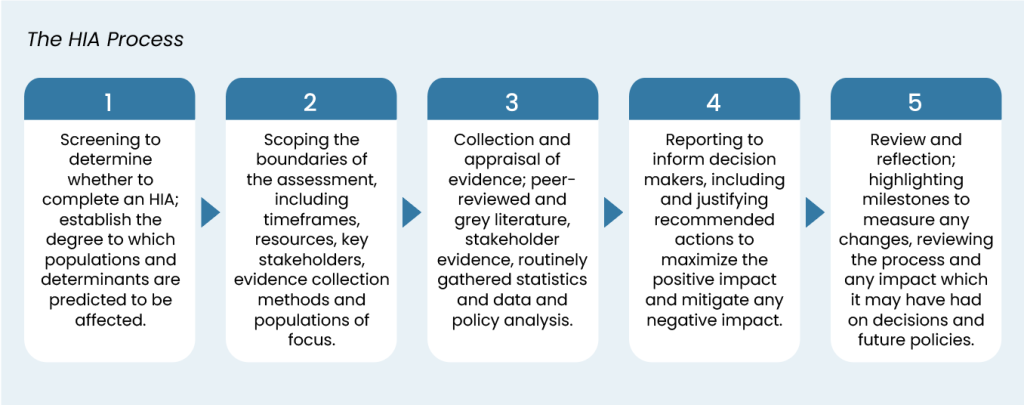
The HiAP approach has been advocated by health experts for some time [4]. Health Impact Assessments (HIAs) are a flexible, rigorous tool which may be a powerful mechanism to embed a HiAP approach [5]. By assessing the distribution of health impacts across population groups, HIA identifies ways to mitigate negative impacts and enhance positive impacts, thus contributing to improving health and reducing inequalities [5]. If done properly, they could unify policy-making to lead to better designed and implemented policies towards healthy lives. Furthermore, HIAs establish a framework for monitoring and evaluating changes in health as part of performance management. Sustainable HIA practice can produce organisational change by promoting transparency and long-term consideration of health in cross-government policy making. The process of HIA, implicitly and explicitly embeds a population health perspective in civil servants across government. The box below outlines the HIA process.
What did we do?
We examined the current state of play with HIAs through discussions with an international group of experts and HIA practitioners, submission of Freedom of Information (FOI) requests to UK ministerial departments, rapid literature review and international comparisons. The research was funded by the Health Foundation.
What did we find?
Freedom of Information requests
Responses to FOI requests across UK government departments revealed limited HIA use:
- 15 departments did not hold the information requested.
- Five departments stated that information on HIAs is not held centrally.
- Three said that they would not be able to answer our request without exceeding the statutory cost limit.
This suggests that although HIA activity may occur sporadically within these departments there is little or no existing ministry level policy, guidance or central documentation. The DHSC were the only department that held information on HIAs. We did not receive any response from one ministerial department.
Literature and case studies
Seven major HIA evaluation reports[7][8][9][10][11][12][13], covering HIAs conducted in the United Kingdom, Australia, New Zealand, North America and Europe between 2002 and 2020 were reviewed. Only a small number of studies evaluated the effectiveness of HIAs in influencing decision making, a high proportion of the HIAs evaluated in these studies were found to be effective [9][11][12]. Some also identified additional benefits arising from HIAs including improved inter-agency collaboration, increased stakeholder engagement and better awareness of health outcomes [7][9][11][12].
Current barriers
Discussions with an expert panel identified the following barriers to HIA and HiAP:
- Absence of dedicated resources and limited capacity
- Absence of a mandatory requirement for HIA
- Limited awareness of health in other impact assessments makes cross-government HiAP challenging
- Ambiguity surrounding competency requirement for HIA practice
- The perception of HIA as an additional burden
- Relative paucity of studies demonstrating HIA effectiveness
The existence of a dedicated health impact assessment support unit can be a key lever to embedding HIA.
Local practice
Local authorities are the main drivers of HIA in England. In London, 55% of local authorities set out a policy requirement for HIA submission as part of a planning application [14]. The London Health Urban Development Unit provides advice and support on assessing the health and wellbeing impacts of development, has developed HIA models, and undertakes HIAs [14]. The Town and Country Planning Association 2019 report specifically recommended the use of HIA in local policy and guidance as a means of planning for health by local authorities [14]. In 2020 Public Health England published guidance for HIA in spatial planning to “provide local authorities the information they need to embed HIA in the local planning system and, in doing so, create safer and healthier places”. Despite support and prominent examples of HIA in local planning, only 30% of local authorities across England mandate its use [15].
International practice
Comparing current HIA practice in Whitehall with the approach of Wales, Scotland, Northern Ireland, Ireland, Australia and New Zealand highlights key differences and provides the chance to learn from what is being done in devolved nations. The consensus amongst experts in the field is that Wales has established a high standard of HIA practice. Members of the expert panel attributed progress in Wales to both enabling legislation and the presence of dedicated long-term support from the Wales HIA Support Unit (WHIASU). WHIASU operates with an equivalent of 3.2 FTE employees, who both undertake HIAs and provide expert knowledge, training, and guidance and HIA frameworks and models to assist external organisations [16]. A notable recurring theme across countries was the vulnerability of HIA support systems to changes in personnel, government leadership and budget cuts to public services.
What next?
Evidence suggests that HIAs are effective in influencing decision making, have wider organisational benefits and instigate a culture of considering health and health inequalities as part of a wider political approach. They represent a mechanism to drive consideration for health and disparities in political decision making. The utility of HIAs will be maximised with dedicated leadership and resource. Furthermore, they should be viewed in the context of a cross-government Health in All Policies Approach.
Recommendations
- Implement a mandatory requirement for HIA in upstream political decision making throughout national government to ensure coherent evidence-informed policy making that prioritises health for all significant policies, strategies, plans and programmes.
- Ensure long-term funded and dedicated Health In All Policy support structure to facilitate health impact assessments across government. Agree national best practice guidance on HIA screening criteria and depth of assessments
- Develop a competency framework to support upskilling of HIA.
- Develop clear guidance to improve consideration of health within other impact assessments.
- Develop capacity for monitoring.
- Progress HIA methodologies such as community engagement and machine learning.
Suggested citation
Lynch H, Holdroyd I, Black D, Cave B, Harris-Roxas B, Haigh F, O’Mullane M, Stevenson A, Vohra S, Ford J. ‘Making Health in All Policies a reality: A call for Health Impact Assessments across government to improve health and address health inequalities’, Evidence Brief, Health Equity Evidence Centre, 2024.
References
- Office for National Statistics. National life tables–life expectancy in the UK: 2018 to 2020. 2021.
- Tinson A, Major A, Finch D. Is poor health driving a rise in economic inactivity? The Health Foundation. 2022.
- Foundation TH. Major study outlines wide health inequalities in England United Kingdom: The Health Foundation; 2015
Available from: https://www.health.org.uk/news-and-comment/news/major-study-outlines-wide-health-inequalitiesin- england - Community and Public Health. Health in All Policies: Ways of Working. 2023.
- Asian Development Bank. Health Impact Assessment: A Good Practice Sourcebook: Asian Development Bank Institute; 2018.
- Green L, Ashton K, Azam S, Dyakova M, Clemens T, Bellis MA. Using health impact assessment (HIA) to understand the wider health and well-being implications of policy decisions: the COVID-19 ‘staying at home and social distancing policy’ in Wales. BMC Public Health. 2021;21(1):1456.
- Bourcier E, Charbonneau D, Cahill C, Dannenberg AL. Peer reviewed: An evaluation of health impact assessments in the United States, 2011–2014. Preventing chronic disease. 2015;12.
- Dannenberg AL. Peer reviewed: Effectiveness of health impact assessments: A synthesis of data from five impact evaluation reports. Preventing chronic disease. 2016;13.
- Haigh F, Harris E, Harris-Roxas B, Baum F, Dannenberg AL, Harris MF, et al. What makes health impact assessments successful? Factors contributing to effectiveness in Australia and New Zealand. BMC Public Health. 2015;15(1):1-12.
- Povall SL, Haigh FA, Abrahams D, Scott-Samuel A. Health equity impact assessment. Health Promotion International. 2013;29(4):621-33
- Rhodus J, Fulk F, Autrey B, O’Shea S, Roth A. A review of health impact assessments in the US: current state-of-science, best practices, and areas for improvement. Cincinnati: Office of Research and Development, National Exposure Research Laboratory, US Environmental Protection Agency. 2013.
- Sohn EK, Stein LJ, Wolpoff A, Lindberg R, Baum A, McInnis-Simoncelli A, et al. Avenues of influence: the relationship between health impact assessment and determinants of health and health equity. Journal of Urban Health. 2018;95:754-64.
- Wismar M, Blau J, Ernst K, Figueras J, WHO. The effectiveness of health impact assessment: scope and limitations of supporting decision-making in Europe: World Health Organization. Regional Office for Europe; 2007.
- Chang M. The State of the Union: Reuniting Health with Planning in Promoting Healthy Communities. In: Association TaCP, editor. 2019.
- Public Health England. COVID-19: review of disparities in risk and outcomes: UK Government; 2020
- Public Health Wales . WHIASU 2001
Available from: https://phwwhocc.co.uk/whiasu/
Related resources
Harnessing Health Impact Assessments for a fairer and healthier future
A healthy population is key to citizen wellbeing, a productive economy and manageable public services. Policy decisions on jobs, income, housing, education, transport and green space have a major impact on health, but do not involve the Department of Health and Social Care. As the government sets out policies to deliver on its manifesto commitments, how can we ensure health is considered across government, mitigating the potential adverse impacts, ensuring equity and accentuating the positives? Here we argue that Health Impact Assessments are a key tool to cross-government action on health and health inequalities.