Seven high-impact interventions to tackle health and care inequalities
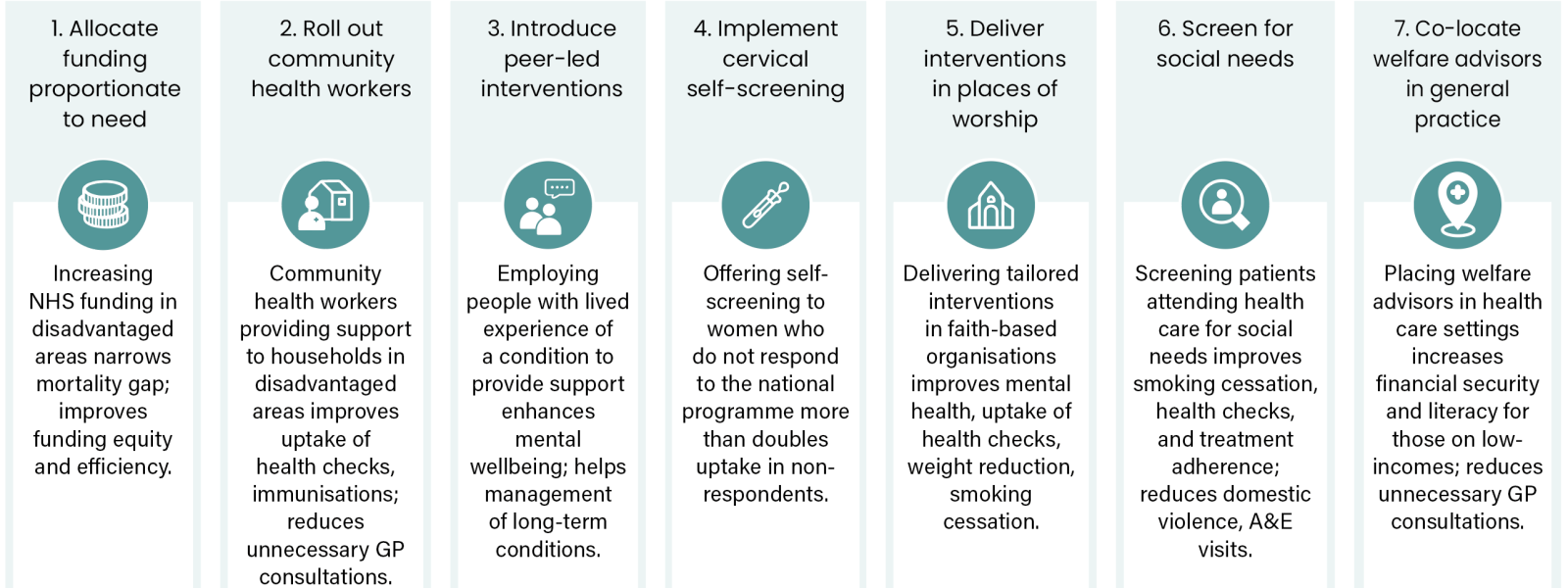
We have undertaken a series of 10 evidence reviews for NHS England and here highlight seven interventions and programmes with the strongest evidence base.
7 high impact interventions[PDF 253kb]
Download documentThere are no silver bullets for addressing health and care inequalities. The key building blocks to develop equity-orientated organisations are inclusive leadership and organisational culture, and multi-component and multi-sector programmes which engage with diverse communities and are sustained over time. Research studies are important in supporting decision makers in understanding the impact of specific interventions or programmes. We have undertaken a series of 10 evidence reviews for NHS England and here highlight seven interventions and programmes with the strongest evidence base.
1. Allocate funding proportionate to need
What is the intervention? Increasing NHS funding to socioeconomically disadvantaged areas.
What does it achieve? Previous research has shown that re-weighting funding formulae to increase funding to socioeconomically disadvantaged areas narrowed the gap in mortality and improved mortality overall. Elsewhere, a recent study found that adjusting the general practice funding formula would enhance both funding equity and efficiency.
Who in the system is best placed to take action? Department of Health and Social Care, NHS England and Integrated Care Boards
Evidence brief: What works: Funding models to address health inequalities
Key papers:
- Barr, B., Higgerson, J., & Whitehead, M. (2014). The impact of NHS resource allocation policy on health inequalities in England 2001-11: Longitudinal ecological study. BMJ, 348, g3231.
- Holdroyd, I., Webster, H., & Smith, A. (2024). Adjusting primary-care funding by deprivation: A cross-sectional study of lower-super-output areas in England. BJGP Open. doi: 10.3399/BJGPO.2024.0185.
2. Roll out community health workers (CHW)
What is the intervention? CHWs visit households in socioeconomically disadvantaged areas to help with barriers to health care, personalised prevention, social support and signposting.
What does it achieve? Previous research found improvements in cancer screening, immunisations, health checks, blood pressure, blood glucose, lipids, physical activity and a reduction in GP consultations.
Who in the system is best placed to take action? Department of Health and Social Care, NHS England, Integrated Care Boards and Local Authorities.
Evidence brief : What works: Community engagement and empowerment to address health inequalities
Key papers
- Hayhoe, B., Petchey, R., & Tait, S. (2018). Integrating a nationally scaled workforce of community health workers in primary care: A modelling study. JRSM, 111(12), 453–461.
- Junghans, C., Murphy, D., & Stewart, S. (2023). Learning from the universal, proactive outreach of the Brazilian Community Health Worker model: Impact of a Community Health and Wellbeing Worker initiative on vaccination, cancer screening, and NHS health check uptake in a deprived community in the UK. BMC Health Services Research, 23(1), 1092.
- Kim, K., Choi, J., & Jung, H. (2016). Effects of community-based health worker interventions to improve chronic disease management and care among vulnerable populations: A systematic review. American Journal of Public Health, 106(4), e3–e28.
- Okasako-Schmucker, M., Farmer, M., & Bensley, J. (2022). Community health workers to increase cancer screening: 3 Community Guide systematic reviews. AJPM, 63(1), 102-110.
- Patil, S. S., White, R., & Steele, M. (2024). Lay advisor interventions for hypertension outcomes: A systematic review, meta-analysis and a RE-AIM evaluation. Frontiers in Medicine, 11, 100036.
- Rana, T., Baptiste, A., & Singh, J. (2023). Effectiveness of community health worker-led interventions in enhancing colorectal cancer screening uptake in racial and ethnic minority populations. Cancer Nursing, 46(1), 54-62.
3. Introduce peer-led interventions
What is the intervention? Peer-led community interventions involve a person who has lived experience of a health condition, or of caring for those with that condition, being employed to use their experiences and empathy to support others.
What does it achieve? Previous research has shown peer-led community interventions improve mental wellbeing, especially for perinatal women, and can help management of long-term conditions.
Who in the system is best placed to take action? Department of Health and Social Care, NHS England, Integrated Care Boards, mental health trusts and Local Authorities.
Evidence brief : What works: Community engagement and empowerment to address health inequalities
Key papers:
- Cooper, R. E., Grewal, M., & Varma, R. (2024). The effectiveness, implementation, and experiences of peer support approaches for mental health: A systematic umbrella review. BMC Medicine, 22(1), 72.
- Huang, R., Lan, Y., & Zhao, T. (2020). Effectiveness of peer support intervention on perinatal depression: A systematic review and meta-analysis. Journal of Affective Disorders, 276, 788-796.
- Lim, G. P., Tan, J. Y., & Teo, S. L. (2024). Peer-led lifestyle interventions for the primary prevention of cardiovascular disease in community: A systematic review of randomised controlled trials. BMC Public Health, 24(1), 812.
- Sokol, R., Fisher, E., & Hill, B. (2016). Peer support for the hardly reached: A systematic review. American Journal of Public Health, 106(7), e1–e8.
- Thompson, D. M., Smith, L., & O’Connor, K. (2022). Peer support for people with chronic conditions: A systematic review of reviews. BMC Health Services Research, 22(1), 427.
4. Implement cervical self-screening
What is the intervention? Offering self-screening to women who do not respond to the national cervical screening programme.
What does it achieve? Self-sampling more than doubled screening uptake in non-respondents, with greater increases among women with lower socioeconomic status. Offering self-testing combined with education through community outreach by health workers had an additional impact, increasing screening uptake by three times in participants from ethnic minority backgrounds or from medically underserved communities.
Who in the system is best placed to take action? Department of Health and Social Care, NHS England, Integrated Care Boards and general practice.
Evidence brief : What works: Improving case finding of long-term health problems in disadvantaged communities
Key papers
- Di Gennaro, G., Cornelius, L., & Salvatori, C. (2022). Does self-sampling for human papilloma virus testing have the potential to increase cervical cancer screening? An updated meta-analysis of observational studies and randomized clinical trials. Frontiers in Public Health, 10, 1003461.
- Sun, C., Kwok, L., & Tung, J. (2023). A systematic review of the cost-effectiveness of interventions to increase cervical cancer screening among underserved women in Europe. European Journal of Health Economics, 24(2), 275-283.
- Yeh, P. T., Kennedy, C. E., & de Vuyst, H. (2019). Self-sampling for human papillomavirus (HPV) testing: A systematic review and meta-analysis. BMJ Global Health, 4(3), e001351.
5. Deliver tailored health interventions in places of worship
What is the intervention? Interventions in faith-based organisations, such as mosques or churches, with tailored education programmes, peer-to-peer health care training, exercise programmes, psychotherapy, smoking cessation and addiction support.
What does it achieve? Previous research has shown improvements in mental health, blood pressure, weight reduction, cancer screening, smoking cessation and engagement with addiction services.
Who in the system is best placed to take action? Department of Health and Social Care, NHS England, Integrated Care Boards and Local Authorities.
Evidence bref: What works: Community engagement and empowerment to address health inequalities
Key papers:
- Abu-Ras, W., Smith, M., & El-Amin, H. (2024). Mosques and public health promotion: A scoping review of faith-driven health interventions. Health Education & Behavior, 51(5), 675-690.
- Chan, K. Y., Patel, R., & Lomba, T. (2023). A systematic review and meta-analysis of the effectiveness of hypertension interventions in faith-based organization settings. Journal of Global Health, 13, 04075.
- Hou, S. I., & Cao, X. (2018). A systematic review of promising strategies of faith-based cancer education and lifestyle interventions among racial/ethnic minority groups. Journal of Cancer Education, 33(6), 1161–1175.
- Sanusi, A., & Thompson, R. (2023). Cardiovascular health promotion: A systematic review involving effectiveness of faith-based institutions in facilitating maintenance of normal blood pressure. PLOS Global Public Health, 3(1), e0001496.
6. Screen for social needs
What is the intervention? Routinely asking patients attending health care, especially general practice, about social needs to provide support or signpost.
What does it achieve? Previous research has found that social needs screening resulted in 1) improved smoking cessation, blood pressure, cholesterol and fruit and veg consumption, 2) increased treatment adherence and immunisations and 3) reduced domestic violence, A&E attendance and hospital readmissions.
Who in the system is best placed to take action? Department of Health and Social Care, NHS England, Integrated Care Boards and general practice.
Evidence brief: What works: Designing health care inclusively for people with low incomes
7. Co-locate welfare advisors in general practice
What is the intervention? Co-locating welfare advisors in health care settings to facilitate access to welfare support.
What does it achieve? Previous research has found that co-located welfare services aimed at people on low incomes, such as co-locating Citizens Advice in general practice, led to improved financial security, increased financial literacy of patients and staff and reduced unnecessary GP attendance.
Who in the system is best placed to take action? Department of Health and Social Care, NHS England, Integrated Care Boards, Local Authorities and general practice.
Evidence brief : What works: Designing health care inclusively for people with low incomes
Key papers:
- Reece, S., Smith, P., & Matthews, J. (2022). A review of the effectiveness and experiences of welfare advice services co-located in health settings: A critical narrative systematic review. Social Science & Medicine, 296, 114746.
- Young D, Bates G. Maximising the health impacts of free advice services in the UK: A mixed methods systematic review. Health Soc Care Community. 2022 Sep;30(5):1713–25.
About this brief
This document has arisen from a series of Evidence Briefs commissioned by NHS England to support their statutory responsibilities to adeliver equitable health care. Policy interventions beyond health care services were not in scope. The views expressed in this publication are those of the Health Equity Evidence Centre and not necessarily those of NHS England or NIHR.
