What works: Community engagement and empowerment to address health inequalities
People from ethnic minority backgrounds and socioeconomically disadvantaged backgrounds experience consistently worse health outcomes than their white British and more affluent counterparts. Statutory guidance has recognised that community engagement and empowerment are vital to reduce these health inequalities. In this evidence brief, we summarise evidence examining the effectiveness of different community-centred strategies to improve health in disadvantaged communities.
What works: Community engagement and empowerment to address health inequalities[PDF 285kb]
Download documentSummary
People from ethnic minority backgrounds and socioeconomically disadvantaged backgrounds experience consistently worse health outcomes than their white British and more affluent counterparts. Statutory guidance has recognised that community engagement and empowerment are vital to reduce these health inequalities, but the processes for achieving these results are less well specified.
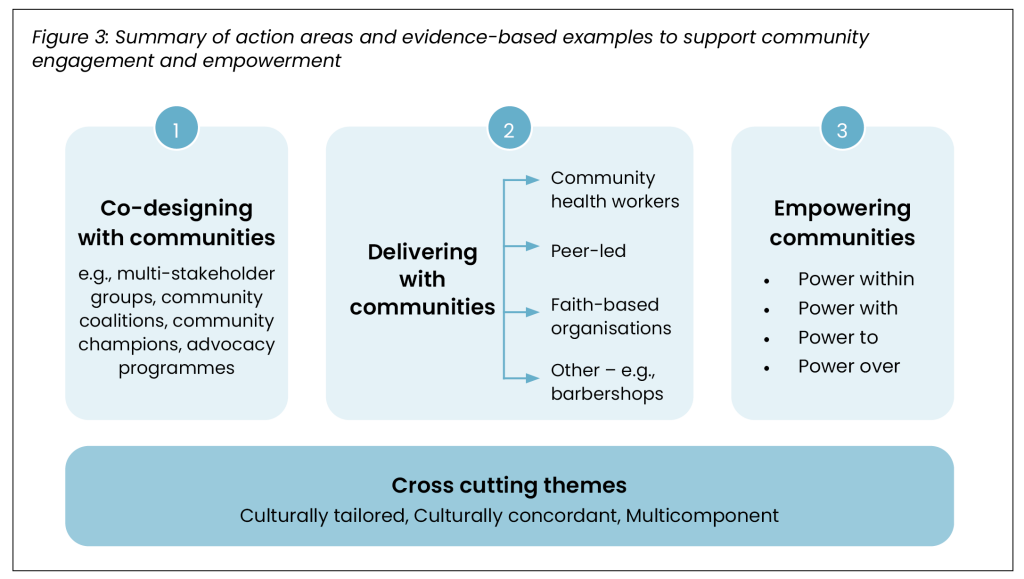
In this evidence brief, we summarise evidence from 32 key research articles examining the effectiveness of different community-centred strategies to improve health in disadvantaged communities. We identified evidence across three categories: co-designing with communities, delivering with communities and empowering communities. The strongest evidence supports the use of Community Health Workers (CHWs) as an interface between health systems and communities, particularly in improving cancer screening uptake and cardiovascular health outcomes. There is also good evidence to support partnerships with faith organisations and community-based peer led support to achieve small but consistent health benefits. Promising early findings demonstrate effectiveness of approaches that seek to partner with communities in the design and delivery of interventions, with examples such as the use of barbershops in the USA to improve health for black men, but the evidence is not sufficient to be conclusive. Cross-cutting themes illustrate that community-centred approaches are more likely to be effective when they are multicomponent and culturally tailored with cultural concordance.
Current challenges
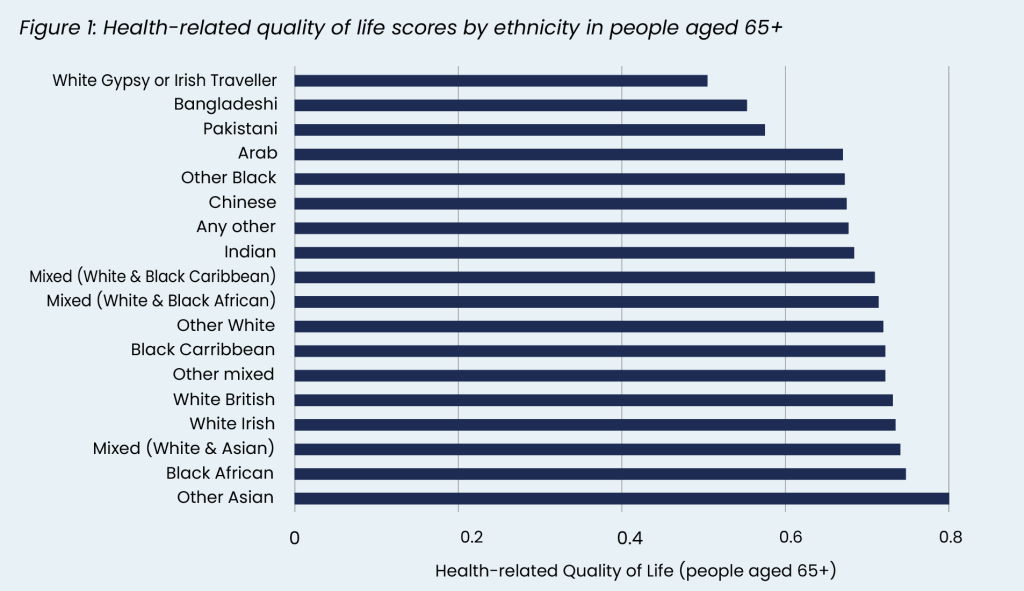
Decades of evidence have highlighted the poor health experienced by disadvantaged communities. White Gypsy or Irish, Bangladeshi, Pakistani and Black Caribbean and African communities have consistently worse health-related quality of life compared to white British communities [1]. Stillbirths and infant mortality are consistently higher in Black African and Caribbean, Pakistani, Indian and Bangladeshi groups [1].
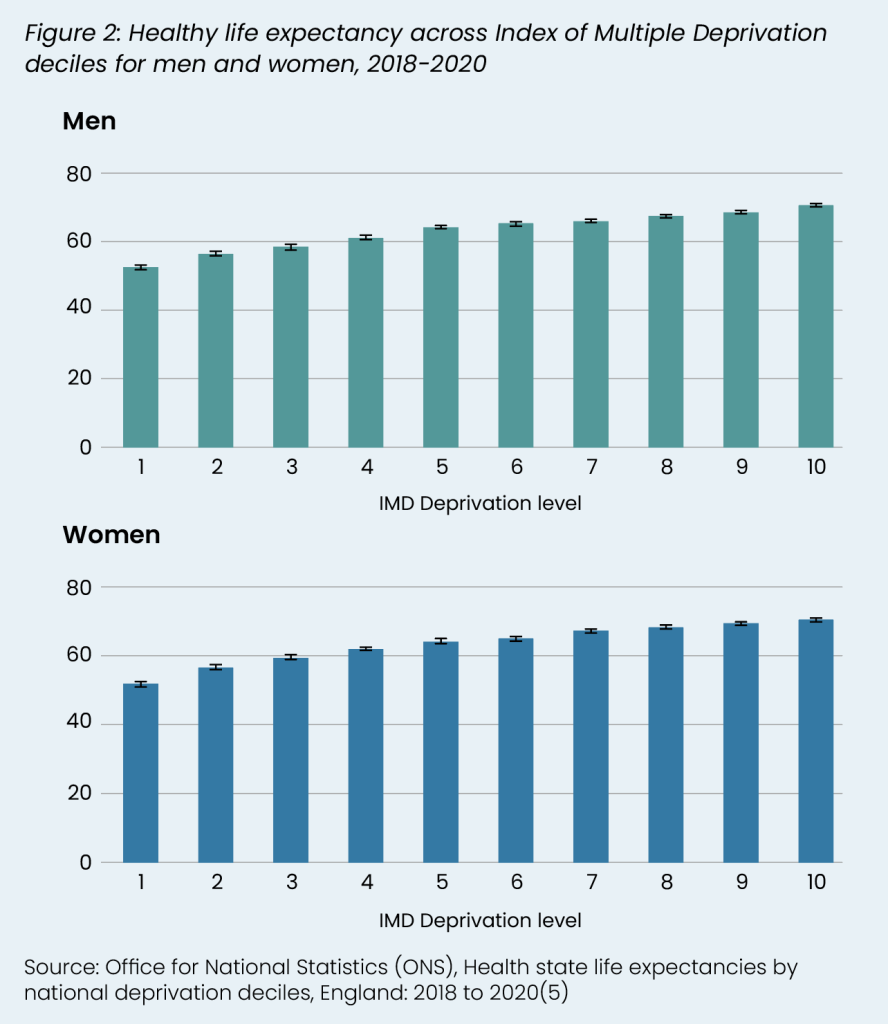
Communities in socioeconomically disadvantaged areas with high rates of poverty also have worse health outcomes. Life expectancy in Bloomfield in Blackpool, the area with the highest deprivation score in England, is 12 years lower for men and 7 years lower for women (68 and 76 in Bloomfield respectively, compared to 80 and 83 in England) [2]. Compared to the England average, it has more children who are obese (30% compared to 23% average for England), more hospital admissions for under 5s (317 per 100,000 compared to 131 in England), and more hospital admissions for self-harm (349 per 100,000 compared to 100 in England) [3].
Disadvantaged communities consistently have poorer access to health care. According to the latest GP Patient Survey, patients from Bangladeshi, Gypsy or Irish Traveller and Pakistani backgrounds reported the least positive overall experience and were the least likely to have their needs met [4].
Community engagement, framed as public involvement, is a Statutory Responsibility for Integrated Care Boards (ICBs), NHS Foundation Trusts and NHS England. Organisations are required to assess the need for, plan and carry out involvement activities, document how it has informed decision-making and have systems in place for reporting. NHS England has produced statutory guidance to support ICBs and other NHS organisations [6], while NICE have published a Community Engagement Quality Standard which sets out recommendations on identifying local priorities, evaluation, identifying community assets and peer and lay roles [7].
The Core20PLUS Connector Programme funds integrated care systems (ICS) to recruit, mobilise and support community connectors to support community engagement and take practical action to improve health and reduce inequalities [8]. There are examples in the UK of Community Health Workers, such as an initiative in Westminster which supports socioeconomically disadvantaged areas through visiting households to identify problems before they escalate [9].
Despite the poor outcomes and statutory responsibilities, local health and care organisations, such as ICBs, trusts and local authorities, can find it difficult to meaningfully engage with communities in the design and delivery of services. There are particular challenges around equitable engagement: people from underserved groups may need more support to participate in engagement work. Involvement payments may support people with financial barriers but also potentially impact on benefits.
Adding to these challenges, community-centred approaches to health and wellbeing, although not novel, have been difficult to conclusively evaluate due to several key barriers. First, by their nature, community-centred approaches must adapt to specific local contexts and, moreover, the process of developing approaches could itself be instrumental to empowerment and health improvement [10]. This granular diversity makes it difficult to draw generalisable findings on effectiveness across studies. Additionally, the intention of community-centred approaches to maximise health, rather than prevent disease, and the tendency to evaluate using experiential and qualitative outcomes, leads to conflict with the established biomedical paradigm in which public health interventions are appraised. Finally, the poor sustainability of community-centred approaches means that long-term outcomes are rarely realised and pose challenges to pooling the findings from across programmes.
Here we seek to summarise the evidence of what works to engage and empower disadvantaged communities.
Summary of evidence
We reviewed 32 research articles identified through the Health Equity Evidence Centre Living Evidence Maps, a complementary search of electronic databases and a snowball search to identify related relevant articles using an AI tool (Litmaps). We prioritise the latest reviews and those of greatest relevance to the UK context. 31 of these articles are systematic reviews or umbrella reviews, while one primary study was included [11] because of its recent contribution to the evidence on use of community-centred approaches in the UK.
The research articles were divided into three broad categories inspired by the review by O’Mara and colleagues examining community engagement to reduce inequalities [12]. We adapted their framework to develop our own categories: 1) Designing with communities, 2) Delivering with communities and 3) Empowering communities (see Figure 3).
1. Community engagement in design
Community engagement in design empowers community representatives to shape policies and interventions, including through coproduction, partnerships and participatory research. Although evidence on its effectiveness is still emerging, the four reviews below indicate that these approaches generally make improvements to health and wellbeing outcomes including access to preventative care and development of culturally sensitive services [13][14][15][16]. Quantifying the added benefit of co-designing services, however, is challenging and has so far been understudied.
The COVID-19 vaccination campaign is a recent success in co-design. Adeagbo and colleagues (2022) reviewed 14 international studies which improved COVID-19 vaccine uptake in black populations [13]. The authors found that communication, community engagement, and culturally inclusive resources significantly improved uptake. UK examples included community champions advising on culturally appropriate processes, languages and support, multi-stakeholder inequalities groups, focus groups in community venues, partnership with faith organisations, and community-informed location of mobile vaccination units and centres [17][18][19]. Conversely, in their international scoping review of 38 studies, Seale and colleagues (2023) found that a lack of engagement with communities in service design was a barrier to uptake of COVID-19 vaccinations [20].
Yip and colleagues’ (2024) review of interventions to reduce ethnic disparities in healthcare in the UK included 29 research articles and examined the evidence at an individual, community and policy level [14]. At a community level, there was evidence that active involvement of underserved patients, families and communities in palliative care service planning promoted culturally appropriate care. An example is the implementation of an Aboriginal health advocacy programme in Australia to support patient involvement in care and negotiating power dynamics [21].
Anderson and colleagues’ (2015) reviewed 58 predominantly USA-based studies which used ‘community coalitions’ to improve partnerships between healthcare organisations and ethnic minority communities [15]. Only one study examined the added value to health from a community coalition model. Wells and colleagues (2013) compared two interventions to improve quality of care for African American people with depression: 1) a co-led community engagement programme; and 2) a train the trainer health care model [16]. The authors found that the community engagement model was more effective at improving health-related quality of life, physical activity, risk factors for homelessness and hospitalisations. Several risks noted, however, were the potential for power imbalances, differences in the knowledge base of community members and professionals, and poor sustainability, which may be counterproductive to empowerment.
2. Community engagement in delivery
Community health workers
Growing evidence demonstrates that community health workers (CHWs) improve health in ethnic minority and low-income populations [22], with the strongest evidence for improvements in cancer screening uptake and reduced cardiovascular disease (CVD) risk factors.
In a systematic review of 61 primarily USA-based studies, for instance, Kim and colleagues (2016) found CHWs delivered significant improvements in cancer screening uptake and cardiovascular health [23]. Most of the 30 studies focusing on cancer screening uptake demonstrated benefits, while, in the 26 studies looking at CVD risk reduction, there were improvements in blood pressure, blood glucose, lipids and physical activity. In the few studies that examined costs, CHWs were found to be cost-effective for breast and cervical cancer screening, blood glucose and hypertension management, particularly when delivered in combination with a professional-led healthcare intervention.
Three reviews focusing specifically on cancer screening generally found beneficial effects. Okasako-Schumucker and colleagues (2022) found 10 to 13 percentage point increases in uptake of breast, cervical and colorectal cancer screening across 76 mostly-USA focused studies, with the largest benefits attained by Asian Americans and people from low-income backgrounds [24]. Similarly, Rana and colleagues’ (2023) meta-analysis of 10 randomised controlled trials found significant increases in colorectal cancer screening uptake in CHW-led interventions [25]. Conversely, a review by Rees and colleagues (2018) which incorporated 15 studies found mixed results for cervical cancer [26].
A recent meta-analysis by Patil and colleagues (2024) found that CHWs effectively reduced blood pressure among adults with hypertension [27]. The review which included 41 studies in disadvantaged populations of low-, middle- and high-income countries, showed that independently delivered CHW programmes led to an average 3.7mmHg decline in systolic and 1.7mmHg decline in diastolic blood pressure relative to a control (for every 10mmHg decline in systolic blood pressure, the risk of major CVD events reduces by 20% [28]).
There is limited evidence on the effectiveness of CHWs for mental health outcomes however. The scoping review by Baskin and colleagues (2021) found only two CHW-led interventions to improve mental health in ethnic minority groups in the UK, with only one of these demonstrating significant improvements in depressive symptoms [29].
The specific effects CHWs have can vary depending on the roles they adopt, such as when acting as navigators, educators or providers of social support. Sharma and colleagues (2019) found that, while all 37 studies of CHWs they reviewed had some beneficial impact, particular roles were better suited to specific objectives [30]. CHWs working as navigators, for instance, were more effective at increasing cancer screening uptake, while education-focused roles tended to better facilitate behaviour change. Rees and colleagues (2018) conclude that a theoretical behaviour change model is important for ensuring that the role a CHW takes on matches the intended outcome [26]. Other reviews find that programmes with multiple components are likely to be most effective at achieving health improvement [25][31], an approach reflected in the UK implementation of the model where CHWs take on a full complement of roles.
UK evidence of community health workers
Junghans and colleagues’ (2023) examined the usefulness of a community-based Brazilian programme in which CHWs visit and build relationships with households, providing opportunities for personalised prevention, support and signposting in a UK context [11]. The programme targeted households in a socioeconomically disadvantaged estate in Westminster who had been visited by a CHW against those who had not yet been visited. After 10 months, 160 households who had been visited by a CHW were 47% more likely to have taken up immunisations, and 84% more likely to have participated in cancer screening and NHS Health Checks respectively, and there were 7.3% fewer unscheduled GP consultations, compared to the 502 households who had not yet been visited (study was not powered to detect statistical significance). Hayhoe and colleagues (2018) have explored the costs and potential outcomes of rolling out the CHW programme nationally [32]. The model assumes coverage of the entire general practice registered population, and finds that for an annual cost of £2.2bn there can be around 1.5 million additional annual cancer screenings (753,000 additional cervical cancer screenings and 482,000 bowel cancer screenings), 20,000 more children per year receiving MMR vaccinations, and improvements in chronic disease management. There was an estimated return on investment of £4 in the most deprived areas of Westminster for every pound invested [33], with a corresponding ROI of £2 for Westminster overall, despite being one of the most affluent boroughs.
Community health workers as patient navigators
CHWs are often employed as health systems navigators, supporting people to understand and access health and social care services such as by addressing language, health literacy, cultural and logistical barriers. We identified five reviews exploring the benefits of patient navigation on health outcomes. Only one of these looked specifically at the use of CHWs in this role, with the remaining reviews including both CHW and professional led navigation.
Five reviews looked at the use of patient navigators in cancer care. All five found that navigation led to significant increases in screening uptake; however, results varied and there were differential effects by race and education. The meta-analysis by Tian and colleagues (2022), for example, which included 15 primarily USA-based trials found that the likelihood of breast cancer screening and diagnosis in women receiving patient navigation doubled when facilitated by patient navigators in ethnic minority and low-income populations [34]. Similarly, in their meta-analysis specifically on the Asian American population, Kim and Han (2022) found navigation increased uptake of screening for a number of cancers [35]. There is also evidence of optimised diagnostic resolution, with Tian and colleagues, for example, finding that navigation shortened the time to diagnosis by an average of 9.9 days. Chan and colleagues’ (2023) umbrella review, meanwhile, found that benefits extended beyond diagnosis, including reduced hospitalisation during treatments, and increased adherence to surveillance appointments, knowledge and patient satisfaction in cancer survivors [31]. Conversely, Mistry and colleagues (2021) reviewed 29 studies examining the role of CHWs as navigators in primary and community care, and found no impact on cancer treatment outcomes [36]. Mosquera and colleagues’ (2023) review demonstrated a risk that patient navigation programmes could widen inequalities in cancer outcomes if not suitably designed and implemented, as indications were that the most affluent groups tend to experience the greatest improvements.
In addition to cancer outcomes, Mistry and colleagues (2021) found evidence for optimised primary care use through use of CHW-led navigation. There was, however, insufficient evidence for impacts on secondary and tertiary healthcare use or clinical outcomes such as blood pressure.
Community health workers as patient educators
CHW as educators focus on health literacy and empowerment through culturally-relevant education, counselling, and signposting. Two recent meta-analyses of CHWs delivering basic medical education and holistic support in people with diabetes have found significant and clinically meaningful impacts on reducing blood glucose (HbA1c) levels. Rawal and colleagues (2021) looked at the effectiveness of lifestyle educational interventions delivered by both peers and CHWs [37]. A sub-group analysis specifically including three CHW-led programmes in the USA and UK showed an average modest decline of 0.18% in HbA1c level. The analysis by Evans and colleagues (2023), meanwhile, included 7 long-duration randomised controlled trials from the USA and Australia and found a larger average 0.5% reduction in HbA1c across underserved study populations, including ethnic minority groups and low-income communities [38].
Community health workers enablers and barriers
Variations in study quality and context-specific factors underlie inconsistencies in CHW effectiveness. Both Kim and colleagues (2016) and Chan and colleagues (2023), for instance, found that variation in the results between specific interventions could be partly explained by differences in the rigour of CHW training, with more advanced training tending to predict improved health outcomes [23][31]. Several reviews also noted that longer study durations tended to be associated with improved outcomes [24][30][31]. However, while Sharma and colleagues (2019) showed that multiple visits are associated with better relationships and better outcomes, a risk is loss to follow-up due to contact fatigue which impacted the outcomes of some studies [30]. In their review of qualitative factors influencing the success of patient navigation programmes, Chan and colleagues (2023) found furthermore that integration with the wider health system was important to achieve sustainability [31].
Faith-based organisations
The faith sector is an important community partner for health improvement and equity, especially for reaching minority groups. We found four systematic reviews that examine the use of faith-based organisations to engage with communities and deliver health-related activities.
Abud-Ras and colleagues (2024) specifically reviewed studies examining mosques for health promotion [39]. Based on 14 studies across six countries, interventions included religiously tailored education programmes, peer-to-peer health care training, exercise programmes, psychotherapy, smoking cessation and methadone maintenance. Most studies were a before-and-after design and there was one RCT. All studies showed favourable results with improvements in mental health, engagement with addiction services, cancer screening and smoking cessation.
Sanusi and colleagues (2023) and Chan and colleagues (2023) both looked at faith-based organisations to deliver cardiovascular programmes [40][41]. Sanusi and colleagues included 24 primary studies which looked at faith-based organisations to deliver cardiovascular health promotion, especially for hypertension [40]. The majority of studies were based in churches in the USA and included six randomised controlled trials. Programmes included health education with direct lifestyle linking, health coaching, diet advice, health measurements and opportunistic blood pressure checks. In a meta-analysis, systolic blood pressure reduced significantly by 3.0 mmHg after 3 months and 0.7 mmHg at 12 months and mean weight reduction at 3 and 12 months of 0.83kg, but there was no significant difference in diastolic blood pressure.
Chan and colleagues (2023) undertook a meta-analysis of 11 studies to examine the overall effect of hypertension interventions in faith-based organisations [41]. All were based in churches in the USA with the exception of one in a Buddhist temple in Thailand. There were a range of interventions, including structured group sessions to promote physical activity or healthy eating, provision of healthy food and walking groups. The authors found a reduction in systolic blood pressure of 6.2 mmHg for people with existing hypertension, but no statistically significant difference for the general population.
A review by Hou and Cao published in 2017 looked at US faith-based interventions for African American, Latino or Hispanic groups to promote cancer prevention [42]. Interventions were all in churches and focused on education, including written material, group education and one-to-one sessions. Faith-based interventions improved knowledge and screening uptake.
The highest quality research on faith-based organisational interventions comes from the USA and is predominantly focused on churches. However more research is taking place in the UK. A recent study from 7 mosques in East London found that presenting health information about bowel cancer in mosques increases the intention to test, recommending it to others and confidence to undertake bowel screening [43]. Overall, there is good evidence of small, but significant, improvements in blood pressure, weight and cancer screening intentions.
Peer-led community interventions
Peer-led community interventions involve a person who has lived experience of a health condition, or of caring for those with that condition, being employed to use their experiences and empathy to support others. We identified ten key reviews which considered community-based peer-led interventions for disadvantaged groups. Four examined mental health, three focused on diabetes, two focused specifically on health inequalities, one on chronic conditions and one on CVD.
The two reviews focused on health inequalities were published in 2015 and 2016 respectively. Harris and colleagues examined if community-based peer support could promote health literacy and reduce inequalities [44]. In this realist review, the authors identified 39 studies relevant to the UK context and found that community-based peer support was likely to be effective when they were based on identifying needs, involving local people in recruitment, using codesign and empowerment education in training, developing partnerships, providing ongoing support and allowing peer support workers autonomy and control. They found that peer support workers best improved health literacy when they have time to engage and create rapport with community members, facilitate social networks and allow community members to be in control and decide what health issues they would like to address.
The second health inequalities review by Sokol and Fisher (2016) examined peer support strategies for the ‘hardly reached’ [45]. In total 44 studies of 47 (94%) showed positive outcomes in terms of engaging and retaining people in health programmes. The authors found that strategies that focused on respect and trust had the greatest engagement, and that benefits were greatest amongst disadvantaged groups.
Of the reviews that focused on mental health, Cooper and colleagues (2024) undertook a review of reviews of peer support approaches for mental health [46]. They explored 25 reviews and found mixed results. There was evidence from meta-analyses that peer support is beneficial in perinatal depression, and mixed evidence for people with severe mental illness. Huang and colleagues (2020), in their meta-analysis of 10 studies found that, in women with perinatal depression, a peer support intervention reduced mean depressive scores (−0.37, 95% CI −0.66 to −0.08). Based on Cooper’s review of reviews key factors of success were adequate training and supervision, recovery-orientated culture in workplace interventions, strong leadership and trusting workplace. Based on three studies which included economic analysis, the authors found peer support was low cost and cost-saving.
Baskin and colleagues (2021) looked at public mental health intervention for minority ethnic groups [29]. Two studies looked at peer support groups for British Pakistani women with depression and an RCT found that it improved social functioning but not depression because, according to complementary focus groups, the intervention was too short and there was resistance from family members.
The final mental health review found mixed results in peer-based health interventions for people with severe mental illness [47]. Based on 18 articles, the authors found that most promising interventions were those that focused on self-management and peer-navigator interventions.
Four reviews explored the use of peer support interventions for chronic diseases finding mixed results on effectiveness. Spencer and colleagues (2024) found that peer support and diabetes self-management education improve diabetes control in a Mayan community in Mexico and in the Korean American, African American, and Latino American communities in the USA [48]. Based on 7 studies, Rawal and colleagues (2020) found that, for diabetes management among migrants and ethnic minorities, peer-led interventions showed relatively better outcomes in terms of HbA1c reduction compared with CHW interventions, but the difference was not statistically significant (p=0.379)[37]. Thompson and colleagues (2022), meanwhile, examined 31 studies in people with chronic conditions and found that peer support was associated with positive, but usually non-significant effects across quality of life and self-efficacy [49]. Lim and colleagues (2024) included two UK feasibility studies examining peer support workers for CVD, reporting challenges in recruitment and retention of peer support workers, especially for disadvantaged groups [50].
Other innovative interventions from the literature – barbershops
Barbershops have been identified as trusted, culturally relevant community spaces and may be opportune locations for the delivery of health promotion services. Khosla and colleagues (2024) published a mini-review of barbershop interventions to address chronic disease [51]. This included two randomised controlled trials in the USA that have looked at improving hypertension in black men through barbershops owned by black men. The BARBER-1 trial included 1297 customers in 17 shops and randomised them to hypertension education coupled with blood pressure monitoring and encouragement / connection to physician care, or a control of blood pressure leaflets. The intervention led to an 8.8% higher hypertension control rate after 10 months and a 21 mmHg reduction in systolic blood pressure for those referred to a hypertension specialist [52]. In the Los Angeles Barbershop Blood Pressure Study, 319 black men in 52 barbershops were randomised to either barbers encouraging customers to see a specialist pharmacist in a barber shop or a control of providing lifestyle advice and doctor appointments [53]. This found a reduction of 22 mmHg in systolic blood pressure in the pharmacist arm compared to control at 6 months. Researchers in the UK are examining similar schemes in hairdressers and beauty therapists [54].
3. Community empowerment
Community empowerment, defined as the process of enabling communities to increase control over their lives, was not explored in any of the studies – most studies aggregate individuals to the community level. A major UK study of community empowerment is the evaluation of the Big Local, a Lottery Funded project which awarded £1million to 150 disadvantaged communities over 10 years and allowed each community to decide how they spent the funds [55]. Each local community established a Big Local Partnership Board with at least 51% residents. There was limited evidence for population-level social or health impacts. The impact on the primary outcome, anxiety, was small and not statistically significant (–0.8 percentage points compared to control, 95% CI –2.4 to 0.7). Similarly, the impacts on the secondary outcomes were small and not statistically significant, with the exception of burglary. However, communities which had moved fastest, measured by spending more than 80% of their grant by 2019/20, had a statistically significant reduction in the composite measure of population mental health. The authors found that the greatest impact was when communities had power within the community, alliances with other agencies, control to make changes and power over other statutory organisations (see table below) [56].
| Power within | Capabilities internal to a community supporting collective control/action. |
| Power with | Capabilities to build alliances and act with others to achieve common goals. |
| Power to | Capabilities to achieve desired ends including establishing structures, procedures and opportunities for collective decisions and actions as well as the outcomes of these. |
| Power over | other institutions or exercise of power over a group of community members by another group. |
Cross-cutting themes
Culturally tailored
A common theme across the studies is the need for culturally tailored interventions for ethnic minority groups. Joo and colleagues (2020) undertook a review of reviews and found that culturally tailored interventions were associated with increased disease knowledge, improved objective clinical outcomes, increased satisfaction and improved access outcomes [57]. This is also supported in our complementary evidence brief exploring interventions to increase uptake, access and use of lifestyle Interventions to address health inequalities.
Yip and colleagues found evidence for culturally adapted education, especially in palliative care [14]. One high quality RCT found that a multilingual online interactive skill-building programme, designed especially for diverse patients and carers using video stories, narratives and testimonials to model how to engage in advanced care planning significantly increased documentation of advanced directives and engagement with advanced care planning, when the intervention was compared with non-culturally adapted easy-to-read advanced directives.
A review of interventions targeting cervical cancer screening found that a key contributor to successful outcomes in 15 studies utilising lay health workers was the adaptation of programmes to be culturally sensitive and specific [26]. For instance, one study by Fang and colleagues (2007) which found a significant increase in uptake among Korean women in the USA, tailored videos used by the lay heath workers so that they were linguistically concordant and modelled contemporary family roles typical of Asian women [58]. However, in the umbrella review by Chan and colleagues (2023), it was found that the success of culturally tailoring patient navigation programmes in cancer care appeared to be dependent on the ethnic group of the target population; cultural tailoring of programmes was effective for groups including Hispanic, Latino and Asian populations but less so for African Americans [31].
Cultural concordance
A pattern throughout the evidence is that interventions which recruited community members from their local community with high cultural concordance were more effective. For example, Murayama and colleagues re-analysed a 6 month RCT in the USA with 164 African American and Latino adults [59]. The authors found that high cultural concordance was associated with greater improvements in Hb1Ac and diabetes self-efficacy compared to those with lower cultural concordance.
Cultural congruence was also commonly cited as a facilitator of success in CHW interventions. Sharma and colleagues (2019), for example, found that, of several factors crucial to the success of CHWs, cultural and linguistic congruence between community health workers and the community was essential to build rapport [30]. Similarly, the umbrella review by Chan and colleagues (2023) found that when patient navigators were from the same community and spoke the same language as the target population it improved trust and increased the success of cancer care outcomes [31].
Multicomponent
The majority of community engagement interventions were multicomponent, including, for example, community health workers, education, navigation, and peer support. It is neither possible, nor desirable, to try to isolate the effects of each component because they often have mutually beneficial effects. This is supported by our complementary evidence brief on increasing the uptake of behavioural interventions for disadvantaged groups that found multifaceted interventions were more likely to address health inequalities.
Further considerations
Community-centred approaches to health are wide-ranging, and inconsistent terminology used in studies means it is possible that our review of the literature was unable to find all relevant reviews. Across all the reviews, a clear majority of the research base is currently based on populations in the USA or low and middle-income countries which may not be translatable to the UK context. This is except for the CHW model which has favourable evidence generated based on implementation in the UK. Due to the range of barriers outlined in the introduction, most of the community-centred approaches looked at in this evidence brief are furthermore understudied which makes drawing conclusions difficult.
What works: key recommendations
| Recommendation | Target audience | GRADE certainty |
| Organisational infrastructure should be established to facilitate involvement with underserved and disadvantaged communities in the design of services, such as community coalitions, advocacy groups and multi-stakeholder partnerships | NHS England, ICBs, PCNs, Trusts, local authorities and GPs | ⊕ ⊕ ⊕
Moderate |
| Community health workers should be used to support underserved communities with preventative services (e.g. cancer screening and immunisations) and chronic disease management (e.g. hypertension and diabetes management). | NHS England, ICBs, PCNs, Trusts, local authorities and GPs | ⊕ ⊕ ⊕ ⊕
High |
| Community health workers should ideally be recruited from the community they serve and provide navigation, health education and social support | NHS England, ICBs, PCNs, Trusts, local authorities and GPs | ⊕ ⊕ ⊕
Moderate |
| Community health worker programmes should be sustained o | NHS England, ICBs | ⊕ ⊕ ⊕
Moderate |
| Health and care organisations should work with faith-based organisations to support screening, immunisation, health promotion and chronic disease management | NHS England, ICBs, PCNs, Trusts, local authorities and GPs | ⊕ ⊕ ⊕
Moderate |
| Community interventions should be culturally tailored, ideally with cultural concordance between staff and residents, and multicomponent | NHS England, ICBs, PCNs, Trusts, local authorities and GPs | ⊕ ⊕ ⊕
Moderate |
| Peer-led community-based interventions should be considered, especially for people with perinatal depression, mental health problems and poor health literacy | NHS England, Local authorities, ICBs | ⊕ ⊕
Low |
| Consider partnering with key community organisations which act as community hubs for underserved communities, such as barbershops, for health promotion and chronic disease management | NHS England, Local authorities, ICBs | ⊕ ⊕
Low |
| Initiatives which seek to empower communities should be designed to increase the power within the community, power with other agency, power to act and power over other organisations to enact change. | NHS England, ICBs, PCNs, Trusts, local authorities and GPs | ⊕ ⊕
Low |
*GRADE certainty communicates the strength of evidence for each recommendation [60].
Recommendations which are supported by large trials will be graded highest whereas those arising from small studies or transferable evidence will be graded lower. The grading should not be interpreted as priority for policy implementation – i.e. some recommendations may have a low GRADE rating but likely to make a substantial population impact.
How this brief was produced
What is the Living Evidence Map on what works to achieve equitable lipid management in primary care?
Using AI-powered software called EPPI-Reviewer, the Health Equity Evidence Centre has developed a Living Evidence Map of what works to address health inequalities in primary care. The software identifies research articles that examine interventions to address inequalities. The evidence map contains systematic reviews, umbrella reviews. More information can be found on the Health Equity Evidence Centre website.
Funding
This Evidence Brief has been commissioned by NHS England to support their statutory responsibilities to deliver equitable health care. Policy interventions beyond health care services were not in scope. DL is funded by NIHR ARC North Thames. The views expressed in this publication are those of the author(s) and not necessarily those of NHS England or NIHR.
Suggested citation
MacDonald H, Martin M, Clark E, Dehn Lunn A, Gkiouleka A, Harasgama S, Lamb D, Ford J. Evidence brief: What works – Community engagement and empowerment to address health inequalities. Health Equity Evidence Centre; 2024
References
- Raleigh V. The Health Of People From Ethnic Minority Groups In England [Internet]. King’s Fund; 2023 May [cited 2024 Aug 23].
Available from: https://www.kingsfund.org.uk/insight-and-analysis/long-reads/health-people-ethnic-minority-groups-england - Public Health England. Health-related quality of life for people aged 65 and over [Internet]. 2023 [cited 2024 Aug 29].
Available from: https://www.ethnicity-facts-figures.service.gov.uk/health/physical-health/health-related-quality-of-life-for-people-aged-65-and-over/latest/#full-page-history - Fingertips | Department of Health and Social Care [Internet]. [cited 2024 Aug 23].
Available from: https://fingertips.phe.org.uk/ - Ipsos MORI. GP Patient Survey National Report 2024 [Internet]. 2024 Jul [cited 2024 Aug 23].
Available from: https://gp-patient.co.uk/surveysandreports - Office for National Statistics. Health state life expectancies by national deprivation deciles, England [Internet]. 2022 [cited 2024 Aug 29].
Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/healthinequalities/bulletins/healthstatelifeexpectanciesbyindexofmultipledeprivationimd/2018to2020 - NHS England,. Working in partnership with people and communities: Statutory guidance [Internet]. 2023 May [cited 2024 Aug 23].
Available from: https://www.england.nhs.uk/long-read/working-in-partnership-with-people-and-communities-statutory-guidance/ - NICE. Community engagement: improving health and wellbeing [Internet]. NICE; 2017 [cited 2024 Aug 23].
Available from: https://www.nice.org.uk/guidance/qs148 - NHS England,. Core20PLUS5 Community Connectors [Internet]. [cited 2024 Aug 24].
Available from: https://www.england.nhs.uk/about/equality/equality-hub/national-healthcare-inequalities-improvement-programme/core20plus5/core20plus5-community-connectors/ - Owolabi B. ‘Saviours’: how community health and wellbeing workers are helping to tackle health inequalities in England [Internet]. NHS England; 2024 Apr [cited 2024 Aug 24].
Available from: https://www.england.nhs.uk/blog/saviours-how-community-health-and-wellbeing-workers-are-helping-to-tackle-health-inequalities-in-england/ - South J, Bagnall AM, Stansfield JA, Southby KJ, Mehta P. An evidence- based framework on community-centred approaches for health: England, UK. Health Promot Int. 2019 Apr;34(2):356–66.
- Junghans C, Antonacci G, Williams A, Harris M. Learning from the universal, proactive outreach of the Brazilian Community Health Worker model: impact of a Community Health and Wellbeing Worker initiative on vaccination, cancer screening and NHS health check uptake in a deprived community in the UK. BMC Health Services Research. 2023 Oct 12;23(1):1092
- O’Mara-Eves A, Brunton G, McDaid D, Oliver S, Kavanagh J, Jamal F, et al. Community engagement to reduce inequalities in health: a systematic review, meta-analysis and economic analysis [Internet]. Southampton (UK): NIHR Journals Library; 2013 [cited 2024 Aug 24]. (Public Health Research).
Available from: http://www.ncbi.nlm.nih.gov/books/NBK262817/ - Adeagbo Morolake Josephine, Olukotun Mary, Musa Salwa, Alaazi Dominic, Allen Upton, Renzaho Andre M. N, et al. Improving COVID-19 Vaccine Uptake among Black Populations: A Systematic Review of Strategies. International Journal Of Environmental Research And Public Health. 2022;19(19):11971–11971.
- Yip JLY, Poduval S, Souza-Thomas L de, Carter S, Fenton K. Anti-racist interventions to reduce ethnic disparities in healthcare in the UK: an umbrella review and findings from healthcare, education and criminal justice. BMJ Open. 2024 Feb 1;14(2):e075711.
- Anderson LM, Adeney KL, Shinn C, Safranek S, Buckner‐Brown J, Krause LK. Community coalition‐driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database of Systematic Reviews [Internet]. 2015;(6).
Available from: https://doi.org//10.1002/14651858.CD009905.pub2 - Wells KB, Jones L, Chung B, Dixon EL, Tang L, Gilmore J, et al. Community- Partnered Cluster-Randomized Comparative Effectiveness Trial of Community Engagement and Planning or Resources for Services to Address Depression Disparities. J GEN INTERN MED. 2013 Oct 1;28(10):1268–78.
- Taplin S, Andrews-Jones B, Chainey A, Das S, Dawson D, Dean A, et al. Mitigating inequalities at a large COVID-19 vaccination centre. Future Healthcare Journal. 2022 Nov 1;9(3):321–5.
- Vanderslott S, Joynes-Burgess K, Kadambari S, O’Dwyer E, Alidu L, Vandrevala T. Examining the role of community champions to promote vaccine uptake in under-served communities in the United Kingdom: Lessons from the COVID-19 pandemic. SSM – Qualitative Research in Health. 2024 Jun 1;5:100436.
- Halvorsrud K, Shand J, Weil LG, Hutchings A, Zuriaga A, Satterthwaite D, et al. Tackling barriers to COVID-19 vaccine uptake in London: a mixed-methods evaluation. J Public Health (Oxf). 2023 Jun 14;45(2):393–401.
- Seale H, Harris-Roxas B, Mustafa K, McDermid P. Communication and engagement of community members from ethnic minorities during COVID-19: a scoping review. BMJ Open. 2023 Jun 1;13(6):e069552.
- Schill K, Caxaj S. Cultural safety strategies for rural Indigenous palliative care: a scoping review. BMC Palliative Care. 2019 Feb 14;18(1):21.
- Anderson LM, Adeney KL, Shinn C, Safranek S, Buckner‐Brown J, Krause LK. Community coalition‐driven interventions to reduce health disparities among racial and ethnic minority populations – Anderson, LM – 2015 | Cochrane Library. [cited 2024 Aug 3];
Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD009905.pub2/full - Kim K, Choi JS, Choi E, Nieman CL, Joo JH, Lin FR, et al. Effects of Community-Based Health Worker Interventions to Improve Chronic Disease Management and Care Among Vulnerable Populations: A Systematic Review. Am J Public Health. 2016 Apr;106(4):e3–28.
- Okasako-Schmucker Devon L, Peng Yinan, Cobb Jamaicia, Buchanan Leigh R, Xiong Ka Zang, Mercer Shawna L, et al. Community Health Workers to Increase Cancer Screening: 3 Community Guide Systematic Reviews. American Journal Of Preventive Medicine [Internet]. 2022;
Available from: https://explore.openalex.org/works/W4312054117 - Rana Tika, Chan Dorothy N. S, Nguyen Khanh T, Choi Chow K, So Winnie K. W. Effectiveness of Community Health Worker-Led Interventions in Enhancing Colorectal Cancer Screening Uptake in Racial and Ethnic Minority Populations. Cancer Nursing [Internet]. 2023;Publish Ahead of Print.
Available from: https://explore.openalex.org/works/W4327555718 - Rees Imogen, Jones Daniel, Chen Hong, Macleod Una. Interventions to improve the uptake of cervical cancer screening among lower socioeconomic groups: A systematic review. Preventive Medicine. 2018;111:323–35.
- Patil Sachin S, Bhayani Vishwa, Yoshida Yilin, Bushweller Leila, Udoh Ekong, Todorov Ivan G, et al. Lay advisor interventions for hypertension outcomes: A Systematic Review, Meta-analysis and a RE-AIM evaluation. Frontiers In Medicine [Internet]. 2024;11.
Available from: https://openalex.org/works/W4398138336 - Ettehad D, Emdin CA, Kiran A, Anderson SG, Callender T, Emberson J, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. The Lancet. 2016 Mar 5;387(10022):957–67.
- Baskin C, Zijlstra G, McGrath M, Lee C, Duncan FH, Oliver EJ, et al. Community-centred interventions for improving public mental health among adults from ethnic minority populations in the UK: a scoping review. BMJ Open. 2021 Apr 1;11(4):e041102.
- Sharma N, Harris E, Lloyd J, Mistry SK, Harris M. Community health workers involvement in preventative care in primary healthcare: a systematic scoping review. BMJ Open. 2019 Dec 1;9(12):e031666.
- Chan RJ, Milch VE, Crawford-Williams F, Agbejule OA, Joseph R, Johal J, et al. Patient navigation across the cancer care continuum: An overview of systematic reviews and emerging literature. CA Cancer J Clin. 2023;73(6):565–89.
- Hayhoe B, Cowling TE, Pillutla V, Garg P, Majeed A, Harris M. Integrating a nationally scaled workforce of community health workers in primary care: a modelling study. J R Soc Med. 2018 Dec;111(12):453– 61.
- Wei C. Bridging the gap: reverse innovation in a deprived London ward to increase community wellbeing and health – a modelling study. Unpublished MPH dissertation. Imperial College London; 2020.
- Tian Lu, Huang Lei, Liu Jie, Li Xia, Ajmal Aisha, Ajmal Maryam, et al. Impact of Patient Navigation on Population-Based Breast Screening: a Systematic Review and Meta-analysis of Randomized Clinical Trials. Journal Of General Internal Medicine. 2022;37(11):2811–20.
- Kim Jinhyun, Han Jina. The effectiveness of patient navigation services in reducing cancer screening disparities among Asian Americans. Ethnicity & Health. 2022;1–15.
- Mistry SK, Harris E, Harris M. Community Health Workers as Healthcare Navigators in Primary Care Chronic Disease Management: a Systematic Review. J Gen Intern Med. 2021 Sep;36(9):2755–71.
- Rawal L, Sahle BW, Smith BJ, Kanda K, Owusu-Addo E, Renzaho AMN. Lifestyle interventions for type 2 diabetes management among migrants and ethnic minorities living in industrialized countries: a systematic review and meta-analyses. BMJ Open Diabetes Res Care. 2021 Apr;9(1):e001924.
- Evans J, White P, Ha H. Evaluating the effectiveness of community health worker interventions on glycaemic control in type 2 diabetes: a systematic review and meta-analysis. Lancet. 2023 Nov;402 Suppl 1:S40.
- Abu-Ras W, Aboul-Enein BH, Almoayad F, Benajiba N, Dodge E. Mosques and Public Health Promotion: A Scoping Review of Faith-Driven Health Interventions. Health Educ Behav. 2024 Aug 5;10901981241252800.
- Sanusi Abayomi, Elsey Helen, Golder Su, Sanusi Osayuwamen, Oluyase Adejoke. Cardiovascular health promotion: A systematic review involving effectiveness of faith-based institutions in facilitating maintenance of normal blood pressure. PLOS Global Public Health. 2023;3(1):e0001496–e0001496
- Chan KY, Srivastava N, Wang Z, Xia X, Huang Z, Poon AN, et al. A systematic review and meta-analysis of the effectiveness of hypertension interventions in faith-based organisation settings. J Glob Health. 2023 Oct 13;13:04075.
- Hou SI, Cao X. A Systematic Review of Promising Strategies of Faith- Based Cancer Education and Lifestyle Interventions Among Racial/ Ethnic Minority Groups. J Canc Educ. 2018 Dec 1;33(6):1161–75
- Waqar S, Yerrakalva D, Duffy TE, Chambers J, Ali Z, Thomas P, et al. Evaluation of a Faith-Placed Health Education Service on Bowel Cancer Screening in Mosques in East London. Health Expectations. 2024;27(4):e70006.
- Harris J, Springett J, Croot L, Booth A, Campbell F, Thompson J, et al. Can community-based peer support promote health literacy and reduce inequalities? A realist review [Internet]. Southampton (UK): NIHR Journals Library; 2015 [cited 2024 Aug 23]. (Public Health Research).
Available from: http://www.ncbi.nlm.nih.gov/books/NBK274412/ - Sokol Rebeccah L, Fisher Edwin B. Peer Support for the Hardly Reached: A Systematic Review. American Journal Of Public Health. 2016;106(7):e1–8.
- Cooper RE, Saunders KRK, Greenburgh A, Shah P, Appleton R, Machin K, et al. The effectiveness, implementation, and experiences of peer support approaches for mental health: a systematic umbrella review. BMC Med. 2024 Feb 29;22(1):72.
- Cabassa LJ, Camacho D, Vélez-Grau CM, Stefancic A. Peer-based health interventions for people with serious mental illness: A systematic literature review. J Psychiatr Res. 2017 Jan;84:80–9.
- Spencer Llinos Haf, Al-Bustami Mahmud, Porter Alison, Naha Gargi, Thomas Rebecca Louise, Rees Siân, et al. Uptake of diabetes follow-up checks by minority community groups: a rapid review of the evidence for the CYMELL study. The Lancet. 2023;402:S86–S86.
- Thompson DM, Booth L, Moore D, Mathers J. Peer support for people with chronic conditions: a systematic review of reviews. BMC Health Serv Res. 2022 Mar 31;22(1):427
- Lim GP, Appalasamy JR, Ahmad B, Quek KF, Ramadas A. Peer-led lifestyle interventions for the primary prevention of cardiovascular disease in community: a systematic review of randomised controlled trials. BMC Public Health. 2024 Mar 14;24(1):812.
- Khosla P, Amin K, Doshi R. Combating Chronic Disease with Barbershop Health Interventions: A Review of Current Knowledge and Potential for Big Data. Yale J Biol Med. 2024 Jun;97(2):239–45.
- Victor RG, Ravenell JE, Freeman A, Leonard D, Bhat DG, Shafiq M, et al. Effectiveness of a barber-based intervention for improving hypertension control in black men: the BARBER-1 study: a cluster randomized trial. Arch Intern Med. 2011 Feb 28;171(4):342–50.
- Victor RG, Lynch K, Li N, Blyler C, Muhammad E, Handler J, et al. A Cluster-Randomized Trial of Blood-Pressure Reduction in Black Barbershops. New England Journal of Medicine. 2018 Apr 5;378(14):1291–301.
- Hair and beauty therapists in London to promote heart health and raise breast cancer awareness [Internet]. 2023 [cited 2024 Aug 28].
Available from: https://arc-sl.nihr.ac.uk/research-and-implementation/our-research-areas/public-health-and-multimorbidity/hair-and-beauty - Popay J, Halliday E, Mead R, Townsend A, Akhter N, Bambra C, et al. Investigating health and social outcomes of the Big Local community empowerment initiative in England: a mixed method evaluation. Public Health Research. 2023 Oct 30;11(9):1–147.
- Popay J, Whitehead M, Ponsford R, Egan M, Mead R. Power, control, communities and health inequalities I: theories, concepts and analytical frameworks. Health Promotion International. 2021 Oct 1;36(5):1253–63.
- Joo Jee Young, Liu Megan F. Effectiveness of Culturally Tailored Interventions for Chronic Illnesses among Ethnic Minorities. Western Journal Of Nursing Research. 2020;43(1):73–84.
- Fang CY, Ma GX, Tan Y, Chi N. A Multifaceted Intervention to Increase Cervical Cancer Screening among Underserved Korean Women. Cancer Epidemiol Biomarkers Prev. 2007 Jun;16(6):1298– 302.
- Murayama H, Spencer MS, Sinco BR, Palmisano G, Kieffer EC. Does Racial/Ethnic Identity Influence the Effectiveness of a Community Health Worker Intervention for African American and Latino Adults With Type 2 Diabetes? Health Education & Behavior. 2017;44(3):485–93.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008 Apr 24;336(7650):924–6.