What works: Finding ways to better support people who frequently attend emergency departments

People who visit emergency departments more frequently than the average often experience multiple socioeconomic difficulties and health problems. In this brief we summarise evidence on how health care services can better support these patients. Meeting these patients’ needs requires an integrated approach that cuts across different health care services but may also involve local authorities and the voluntary sector.
What works: Finding ways to better support people who frequently attend emergency departments[PDF 200kb]
Download documentSummary
People who visit emergency departments more frequently than the average often experience multiple socioeconomic difficulties and health problems. Evidence shows that these patients cannot have their needs sufficiently met in emergency departments and they are likely to have much higher mortality rates than the general population.
In this brief we summarise evidence from 46 studies on how health care services can better support these patients. The findings show that meeting these patients’ needs requires an integrated approach that cuts across different health care services but may also involve local authorities and the voluntary sector. The main components of such an approach include:
- screening tools combined with clinical judgement to identify patients at risk
- good primary care access and continuity
- integrated multidisciplinary services
- a whole-person approach.
Current challenges
High intensity use of Emergency Departments (ED) is most commonly defined as using these services five or more times per year [1]. People who visit ED more frequently than the average are usually people who experience complex socioeconomic disadvantage and at the same time suffer from multiple physical and mental health conditions [2] They are likely to deal with complex problems like housing insecurity, drug and alcohol issues, social isolation and poverty. Emergency services are often not well placed to address these patients’ needs, resulting in them feeling unheard and potentially reluctant to engage in healthcare services more widely [1]. Alarmingly, UK data shows that people who attend ED frequently and especially those aged 30 to 49 have much higher mortality rates than their peers in the general population [1]. Identifying these patients and providing them with more effective support is a challenge.
The NHS has set up a dedicated High Intensity Use programme to support the coordination of local health and social care systems as providers of a more holistic type of care that can effectively meet the complex needs of these patients. Within this approach primary care and general practice services are key partners. It has been shown that frequent use of GP services can be an early warning sign of high intensity ED use. Therefore, general practice can contribute to a preventive approach through the identification of patients at risk but also to the provision of a more comprehensive health care. In the following section, we discuss evidence on how health care services can better support people who frequently attend emergency departments.
Summary of evidence
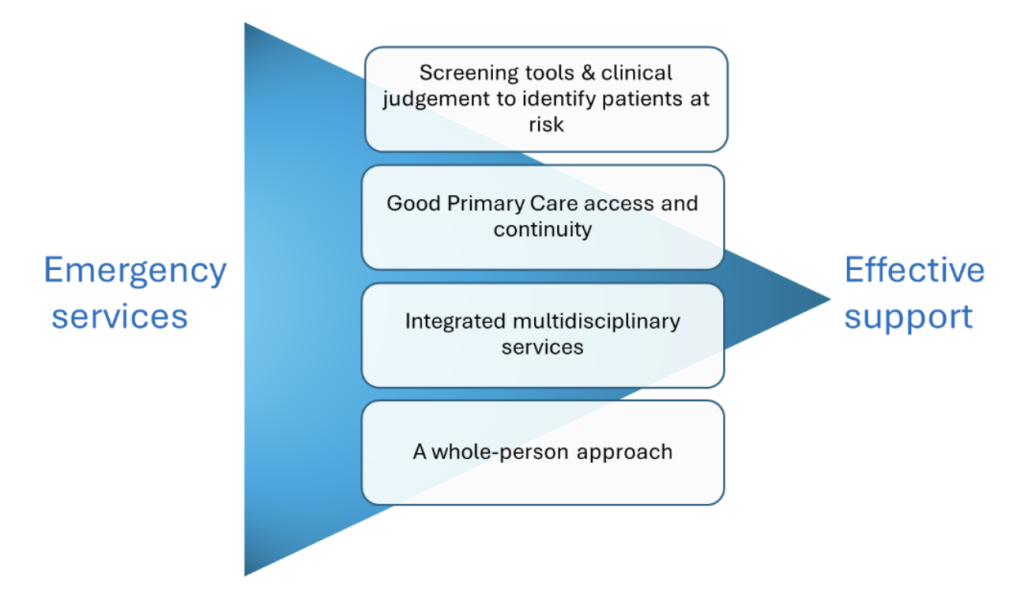
Using our evidence maps and complementary searches for grey literature, we identified 46 studies exploring what works in better supporting people who frequently attend emergency departments. Nineteen studies were either a systematic or a rapid review and twenty-seven were primary studies. Overall, the evidence suggests that to better support people who frequently attend emergency departments, we need an integrated approach that cuts across different health care services but may also involve local authorities and the voluntary sector. As shown in Figure 1, this approach involves four key action points:
-
- Screening tools combined with clinical judgement to identify patients at risk
- Good primary care access and continuity
- Integrated multidisciplinary services
- A whole-person approach
1. Screening tools combined with clinical judgement to identify patients at risk
There is substantial evidence suggesting that frequent use of emergency services is associated with health inequalities [3]. This means that people who use these services more frequently are more likely to live in socioeconomically disadvantaged areas and have complex physical and psychosocial needs. In such contexts, finding the individuals who are likely to visit emergency services at higher rates than the average requires a proactive approach and combined use of quantitative and qualitative information [4].
A scoping review of screening tools to identify patients with complex health needs at risk of high use of health care services aimed to identify a short, valid screening tool for adult populations of all ages [5]. They originally identified 14 tools out of which nine targeted older patients and five targeted adult patients of all ages. Most were lengthy and only IM-SA, a self-administered questionnaire, can be completed in less than 15 minutes. A more extensive questionnaire is included in the INTERMED tool which addresses biological, psychological, social, and healthcare domains, but it must be observer-rated and takes between 20 and 30 minutes. Finally, one tool (Homeless Screening Risk of Re-Presentation) was identified as an effective predictor of health care services use among homeless people only. The authors concluded that IM-SA is a short, reliable and well-validated screening tool which has the potential to identify patients at risk of frequent health care use and further research is required to determine its usefulness.
The context where screening tools can be administered varies between the emergency and primary care services. There is a lack of evidence exploring whether such tools are differentially effective for people who have already been identified (e.g. by ED use) and those who are likely to become frequent users. However, evidence suggests that identifying patients also requires in-depth contact between health practitioners and patients either through community-based outreach activities or within primary care and general practice services [4][6]. A systematic review of twenty studies on the characteristics of effective case management in primary care showed that the clinical judgment of health care providers is crucial for successful case-finding [4]. The study discussed how practitioners, by just exploring patients’ complex care needs (e.g., combination of physical, psychiatric, and social conditions; poverty, polypharmacy, or lack of social support), can make valid assessments about who is likely to need additional support that will prevent them from inappropriately seeking care at emergency departments. Additional evidence from a study conducted in the US suggests that understanding which are the commonest complaints that lead to repeat visits to emergency services (e.g. chest pain or shortness of breath) might provide practitioners with additional guidance during the case-finding process [7].
2. Good primary care access and continuity
Primary care services emerged as an important part of effective approaches in the support of people who frequently attend emergency departments. A systematic review of interventions reducing frequent visits to the ED [8] found that primary care professionals and co-ordinated access to primary care resources were part of different models of integrated care including case management, personalised care plans, and information sharing across health care services. A systematic review of 48 observational studies describing potential factors influencing ED visits and hospital admissions found that better access and continuity of care reduce unscheduled secondary care use [9]. Specifically, ED attendance is reduced when people can see the same GP every time they visit their practice and when practices can be accessed beyond regular working hours [10]. The evidence points to the same direction regarding emergency hospital admissions in studies conducted in the US and Canada.
Another systematic review focused on the effects of continuity of care on health outcomes among patients with diabetes mellitus and/or hypertension. Based on 42 included studies, the review showed that continuity in primary care associated with reduced hospitalisation, emergency room attendances, healthcare expenses but also with reduced disease related complications and mortality rates [11]. Having a primary care doctor and greater continuity of care with them were both also associated with reduced emergency department use in a cross-sectional study in Canada. The study used information from a random sample of 95,173 people aged 65 years or more living in Quebec [12].
Finally, three primary studies from the UK [13] US [14] and Canada [15] highlighted that it is not only the actual features of primary care that impact emergency services use but people’s perceptions of primary care. Specifically, their findings show that when patients perceive primary care as ineffective or poor in terms of telephone access, inability to get appointments or shorter opening hours they are more likely to turn to emergency departments [9].
3. Integrated multidisciplinary services
The evidence highlights that a holistic approach in the care provided to people who frequently use emergency services requires multidisciplinary teams that involve different services and providers. The most studied example of such an approach is that of case management [6]. Overall, evidence shows that case management can reduce emergency department attendance and unplanned hospital admissions. However, the range of effect varies depending on population and context and the methodology used in the reviewed studies [6][8][16][17].
Case management is a multidisciplinary approach used to assess, plan, facilitate and coordinate care to meet patient needs [18]. The evidence shows that interdisciplinary case management teams often include a case manager together with primary care providers, substance abuse counselling or referral services, assistance with financial entitlements [6][16], psychologists, social workers, and/or housing and community resource liaisons [8][16].
Despite the heterogeneity of studied interventions and findings, certain features of case management emerged as crucial for its effectiveness in supporting people outside emergency departments. These include engaging patients and considering their objectives and goals, frequent in-person contacts and liaison with social resources, effective communication and relationships between case managers and primary care providers, and a systemic approach to care [4][18][19]. A synthesis of interventions targeted to frequent users with complex needs highlighted the importance of training the case managers with low caseloads, involving peers and promoting self-management skills [20].
Further, a systematic review showed that the intensity of case management correlates with improved emergency department outcomes. Intensity refers to frequency of follow up, and an assertive and persistent outreach to assist patients in attending their appointments [6]. However, one of the studies included in the review suggests that the range of reduction in ED attendance depends on patient level of prior ED use, with those with higher levels of prior ED use (>20 visits a year) continuing to use the ED more than those with lower levels of prior use (5–11 visits a year) [21]. Given that a multidisciplinary intervention like case management frequently implies a significant cost, it might be more effective and cost-efficient to have a differential approach regarding the level of intensity according to patients’ profiles [22]. Evidence on cost-effectiveness is still mixed as many studies report reduction of mainly ED costs and less of inpatients costs, the study design is often weak and usually the analysis does not consider the cost of the case management intervention. It is likely that savings from ED or hospital costs are counterbalanced by an increase in the cost of such programmes [6][22][23][24][25][26].
Another example of interdisciplinary care is personalised care plans. Care plans interventions often involved multifaceted assessment of the health and social needs of patients to guide future care decisions [16]. However, contrary to case management, they were described as involving a limited number of services and providers and being delivered without a designated case manager [8]. Evidence regarding the impact of individualised care plans on reducing emergency attendance among frequent users suggests that it also leads to a reduction in ED visits. However, the extent to which this is significantly different from other forms of care needs further assessment [16]. Studies on individualised care plans report savings that mostly come from reduced ED costs [8][16]
More examples of interdisciplinary care come from literature focusing on older people, one of the two most common age groups along with people aged 20 to 29 to attend emergency services more frequently [1]. A review of interventions to reduce unplanned admissions of care home residents showed that integrated care and quality improvement programmes providing additional support to care homes (e.g. the English Care Homes Vanguard initiatives) can reduce unplanned admissions [27]. However, the specificities of each intervention should be decided according to the context and considering the short-term and long-term cost-effectiveness. The study showed that most studies reported cost savings, but weak study designs and limited reporting meant that findings should be interpreted with caution.
Finally literature on homeless populations who are also among the most common groups of frequent users [1] shows a slightly different image. A systematic review of case management interventions for the homeless, vulnerably housed and persons with lived experience showed that it is only interventions with greater intensity like intensive case management, assertive community treatment and critical time intervention that associate significantly with reductions in the number of emergency department visits and days in hospital [25]. The review included 56 primary studies and showed that intensive approaches also reduce substance use, improve housing stability and increase access to financial assistance. The study concluded that intensive case management for these groups is likely to be cost-effective when all costs and benefits to society are considered.
4. A whole-person approach
As shown by the examples discussed in the above section, different populations require different approaches. Frequent users of emergency services are patients with multiple, complex needs and therefore adopting a whole-person approach is necessary to meet patients’ needs. According to the reviewed literature, adopting a whole-person approach requires addressing patients’ health and social care needs and addressing barriers in accessing appropriate care. For example, a US study conducted a retrospective cohort analysis of patterns of frequent ED use among 4087 patients [7]. Abdominal pain, chest pain, and shortness of breath were the leading complaints and the leading sources of hospital admissions and repeat visits. Chart review in this study showed that it was difficult to define whether high utilisation for these three complaints was more related to medical conditions or to social-behavioural factors instead of being an outcome of the interplay between the two.
According to evidence, engaging patients in individualised care plans or case management models, addressing their own health objectives, and facilitating their connection with informal support networks are key for the success of integrated care interventions [18][19]. Further, the frequency of prior use of emergency service might require different levels of intervention intensity.
Addressing social determinants of health which drive the increased care demand and set barriers in accessing appropriate care is also needed. Evidence shows that interventions targeted to chronically ill homeless adults which combine case management with housing offers/arrangements result in fewer hospital days and emergency department visits compared with usual care [28]. Further, interventions addressing housing consistently lead to improvements in this area too [16].
Finally, a study conducted by the Institute of Fiscal Studies in 2018 [29] highlighted that reductions in social care spending for individuals aged 65 and above have resulted in increased emergency service usage, evidenced by both a higher average number of visits per resident and an increased number of unique patients visiting ED annually. Although we lack evidence on whether social care provision reduces emergency services utilisation among frequent users, findings like those produced by the Institute confirm that addressing patient social needs should be part of an effective strategy.
Transferable evidence
The evidence around the integration of multidisciplinary services and providers is aligned with the transferable evidence from the EQUALISE study. Specifically, it highlights the importance of connectedness as a guiding principle of equitable primary care and the need to incorporate multidisciplinary care in organisational practices across primary care [30]. Further, the evidence around a personalised approach that addresses patient social needs is aligned with the EQUALISE framework which suggests that addressing patient life conditions should be a prioritised area of action. This evidence also echoes the recommendations of the FAIRSTEPS study for adopting a locally sensitive approach for the identification of the patients harmed by inequity and their problems in accessing services [31].
Limitations
Evidence discussed in this brief comes mostly from reviews that adopt different or unspecified definitions of frequent use. Therefore, it does not offer enough guidance in terms of the differential impact that interventions have on frequent users according to their level of use. Due to the heterogeneity of studies and their findings we decided to focus on emergency services attendance as our main outcome. However, conclusions might slightly differ if we consider additional outcomes such as (re)hospitalisation, and length of hospital stay or if we look at different types of emergency services. Due to our emphasis on primary care, we did not conduct a review of interventions outside primary care which explicitly focus on addressing the social determinants of health and patient social needs. However, the findings discussed highlight that this is an additional area of action and possibly further research.
What works: Key recommendations
The Grading of Recommendations, Assessment, Development and Evaluations (GRADE) [32] framework has been adopted to grade the quality of the evidence and support recommendations.
| Recommendation | Target audience | GRADE certainty |
| Combine quantitative tools and practitioners’ assessment to identify patients at risk in primary care. | Practices/ ICBs | ⊕ ⊕
Low |
| Ensure that people at risk of frequently attending the ED have good access to continuity of care (i.e. a single health professional or team who provide care). | Practices | ⊕ ⊕ ⊕ ⊕
High |
| Consider case management for people who frequently attend the ED with adequate monitoring and evaluation. | Practices/PCNs/ ICBs | ⊕ ⊕
Low |
| Undertake care planning for people with complex health and care needs who are at risk of unplanned hospital attendance and admissions. | Practices/PCNs | ⊕ ⊕
Low |
| Build multidisciplinary teams to support the social needs of frequent users, such as housing and welfare. | Practices/PCNs/ ICBs | ⊕ ⊕
Low |
| Consider community-based outreach activities to provide proactive care to communities facing significant disadvantage, such as people who are homeless, care home residents and those with alcohol and drug addiction. | PCNs/ ICBs | ⊕
Very low |
| Build integrated services and patient pathways with primary care, local authorities and the voluntary and community sector to help patients with complex needs to receive the support they need. | Practices/PCNs/ ICBs | ⊕ ⊕
Low |
Useful links
Summary of how the brief was produced
What is the Living Evidence Map on What Works to address health inequalities in primary care?
Using AI-powered software, called EPPI-Reviewer, the Health Equity Evidence Centre has developed a Living Evidence Map of what works to address health inequalities in primary care. The software identifies research articles which examine interventions to address inequalities. The evidence map contains systematic review and umbrella reviews. More information can be found on the Health Equity Evidence Centre website.
Suggested citation
Gkiouleka A, Dehn Lunn A, Ford J. ‘What works – Finding ways to better support people who frequently attend emergency departments’, Evidence Brief, Health Equity Evidence Centre; 2024.
References
- British Red Cross. Nowhere else to turn. Exploring high intensity use of Accident and Emergency services [Internet]. 2021 Nov [cited 2024 May 13]
Available from: https://aace.org.uk/wp-content/uploads/2021/11/hiu-report-final.pdf - NHS England » High Intensity Use programme [Internet]. [cited 2024 Jun 6].
Available from: https://www.england.nhs.uk/high-intensity-use-programme/ - How do population, general practice and hospital factors influence ambulatory care sensitive admissions: a cross sectional study | BMC Primary Care [Internet]. [cited 2024 Jun 7]
Available from: https://link.springer.com/article/10.1186/s12875-017-0638-9 - Hudon C, Chouinard MC, Pluye P, El Sherif R, Bush PL, Rihoux B, et al. Characteristics of case management in primary care associated with positive outcomes for frequent users of health care: a systematic review. The Annals of Family Medicine. 2019;17(5):448–58.
- Marcoux V, Chouinard MC, Diadiou F, Dufour I, Hudon C. Screening tools to identify patients with complex health needs at risk of high use of health care services: A scoping review. PLOS ONE. 2017 Nov 30;12(11):e0188663.
- Kumar GS, Klein R. Effectiveness of Case Management Strategies in Reducing Emergency Department Visits in Frequent User Patient Populations: A Systematic Review. The Journal of Emergency Medicine. 2013 Mar 1;44(3):717–29.
- Hardy M, Cho A, Stavig A, Bratcher M, Dillard J, Greenblatt L, et al. Understanding Frequent Emergency Department Use Among Primary Care Patients. Population Health Management. 2018 Feb;21(1):24–31.
- Soril LJJ, Leggett LE, Lorenzetti DL, Noseworthy TW, Clement FM. Reducing Frequent Visits to the Emergency Department: A Systematic Review of Interventions. PLOS ONE. 2015 Apr 13;10(4):e0123660.
- Huntley A, Lasserson D, Wye L, Morris R, Checkland K, England H, et al. Which features of primary care affect unscheduled secondary care use? A systematic review. BMJ Open. 2014 May 1;4(5):e004746.
- Van Uden C, Crebolder H. Does setting up out of hours primary care cooperatives outside a hospital reduce demand for emergency care? Emergency Medicine Journal. 2004;21(6):722–3.
- Chan KS, Wan EYF, Chin WY, Cheng WHG, Ho MK, Yu EYT, et al. Effects of continuity of care on health outcomes among patients with diabetes mellitus and/or hypertension: a systematic review. BMC Fam Pract. 2021 Jul 3;22(1):145.
- Ionescu-Ittu R, McCusker J, Ciampi A, Vadeboncoeur AM, Roberge D, Larouche D, et al. Continuity of primary care and emergency department utilization among elderly people. CMAJ. 2007 Nov 20;177(11):1362–8.
- Baker R, Bankart M, Rashid A, Banerjee J, Conroy S, Habiba M, et al. Characteristics of general practices associated with emergency-department attendance rates: a cross-sectional study. BMJ quality & safety. 2011;20(11):953–8.
- Cheung PT, Wiler JL, Ginde AA. Changes in barriers to primary care and emergency department utilization. Archives of Internal Medicine. 2011;171(15):1393–400.
- McCusker J, Tousignant P, Da Silva RB, Ciampi A, Lévesque JF, Vadeboncoeur A, et al. Factors predicting patient use of the emergency department: a retrospective cohort study. Cmaj. 2012;184(6):E307–16.
- Moe J, Kirkland SW, Rawe E, Ospina MB, Vandermeer B, Campbell S, et al. Effectiveness of Interventions to Decrease Emergency Department Visits by Adult Frequent Users: A Systematic Review. Academic Emergency Medicine. 2017;24(1):40–52.
- Iovan S, Lantz PM, Allan K, Abir M. Interventions to Decrease Use in Prehospital and Emergency Care Settings Among Super-Utilizers in the United States: A Systematic Review. Med Care Res Rev. 2020 Apr 1;77(2):99–111.
- Hudon C, Chouinard MC, Lambert M, Dufour I, Krieg C. Effectiveness of case management interventions for frequent users of healthcare services: a scoping review. BMJ Open. 2016 Sep 1;6(9):e012353.
- Hudon C, Chouinard MC, Lambert M, Diadiou F, Bouliane D, Beaudin J. Key factors of case management interventions for frequent users of healthcare services: a thematic analysis review. BMJ open. 2017;7(10):e017762.
- Bodenheimer T, Berry-Millett R. Care management of patients with complex health care needs. Policy. 2009;1(6):1–16.
- Shumway M, Boccellari A, O’Brien K, Okin RL. Cost-effectiveness of clinical case management for ED frequent users: results of a randomized trial⋆. The American journal of emergency medicine. 2008;26(2):155–64.
- Lee JY, Muratov S, Tarride JE, Holbrook AM. Managing High-Cost Healthcare Users: The International Search for Effective Evidence-Supported Strategies. Journal of the American Geriatrics Society. 2018;66(5):1002–8.
- Joo J y., Liu M f. Case management effectiveness in reducing hospital use: a systematic review. International Nursing Review. 2017;64(2):296–308.
- Di Mauro R, Di Silvio V, Bosco P, Laquintana D, Galazzi A. Case management programs in emergency department to reduce frequent user visits: a systematic review. Acta Biomed. 2019;90(Suppl 6):34–40.
- Ponka D, Agbata E, Kendall C, Stergiopoulos V, Mendonca O, Magwood O, et al. The effectiveness of case management interventions for the homeless, vulnerably housed and persons with lived experience: A systematic review. PLOS ONE. 2020 Apr 9;15(4):e0230896.
- Stanton A, Osoteo K. Effect of Case Management on Frequency of Emergency Department Visits by Persons with Mental Illness: A Systematic Review. Williams Honors College, Honors Research Projects [Internet]. 2016 Jan 1
Available from: https://ideaexchange.uakron.edu/honors_research_projects/245 - Chambers D, Cantrell A, Preston L, Marincowitz C, Wright L, Conroy S, et al. Reducing unplanned hospital admissions from care homes: a systematic review. Health Soc Care Deliv Res. 2023 Oct;1–130.
- Sadowski LS, Kee RA, VanderWeele TJ, Buchanan D. Effect of a Housing and Case Management Program on Emergency Department Visits and Hospitalizations Among Chronically Ill Homeless Adults.
- Crawford R, Stoye G, Zaranko B. The impact of cuts to social care spending on the use of Accident and Emergency departments in England [Internet]. The IFS; 2018 Jun [cited 2024 May 14].
Available from: https://www.ifs.org.uk/uploads/publications/wps/WP201815.pdf - Gkiouleka A, Wong G, Sowden S, Bambra C, Siersbaek R, Manji S, et al. Reducing health inequalities through general practice. The Lancet Public Health. 2023;8(6):e463–72.
- Jackson B, Ariss S, Burton C, Coster J, Reynolds J, Lawy T. The FAIRSTEPS Study: Framework to Address Inequities in pRimary care using STakEholder PerspectiveS—short report and user guidance. 2023.
- Siemieniuk R, Guyatt G. What is GRADE. BMJ J Best Practice. 2019;10:77–85.