What works: Health and care interventions to support people from disadvantaged backgrounds with musculoskeletal conditions

17.1 million people in England are estimated to be living with a musculoskeletal (MSK) condition. This evidence brief explores what health and care interventions work to improve outcomes for people from disadvantaged backgrounds, and what approaches are most effective in addressing the inequalities they face.
What works: Health and care interventions to support people from disadvantaged backgrounds with MSK conditions[PDF 324kb]
Download documentSummary
Over 20 million people are affected by musculoskeletal (MSK) conditions in the UK. Women, people from a minority ethnic background and those living in a socioeconomically disadvantaged area report higher rates of MSK problems. Low back pain is the leading cause of years lived with disability (YLDs) in the UK with chronic pain predicted to grow in prevalence by 32% by 2040 due to an ageing population with multiple long-term health conditions. Obesity and mental health problems are also more prevalent in disadvantaged communities compounding MSK problems.
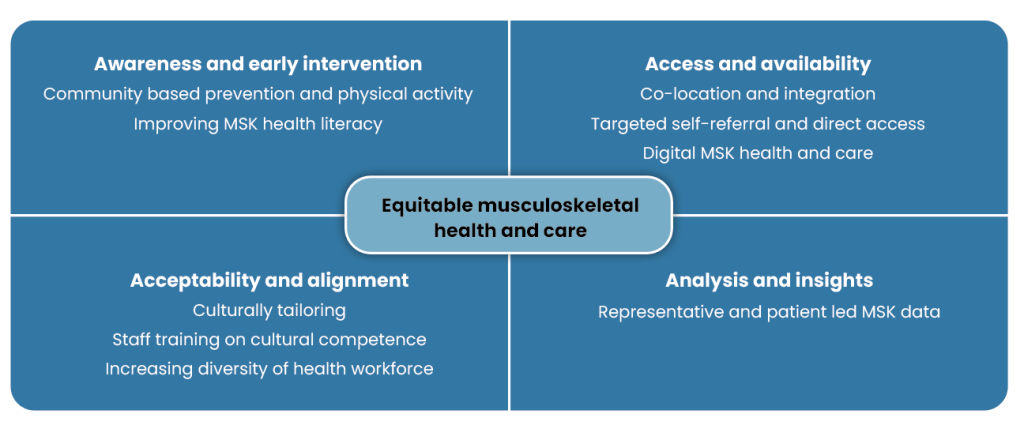
Previous research shows that MSK services do not meet the needs of underserved groups, and the evidence describing what works to address these inequalities is limited. However, the evidence that does exist suggests that care for people with MSK conditions can be made more equitable through:
- Awareness and early intervention, with prevention approaches such as physical activity being delivered at community level to improve MSK health with bespoke interventions to improve health literacy.
- Access and availability of integrated services, targeted self-referral and direct access pathways, and digital MSK tools.
- Acceptability and alignment of services to diverse groups through cultural tailoring of interventions, improving staff cultural competency and increasing diversity of the workforce.
- Analysis and insights of MSK data through an equity-lens by having representative and patient-led data to drive service delivery.
Current challenges
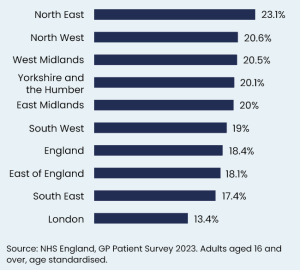
17.1 million people in England are estimated to be living with an MSK condition [1]. In 2023, 18.4% of people reported having a long-term MSK problem, an increase from 17.6% in 2022 [2]. Based on data from the GP Patient Survey in 2023, the prevalence of self-reported MSK conditions was higher in females (20.9%) than in males (15.8%) and in the North East of England (Figure 1) [3].
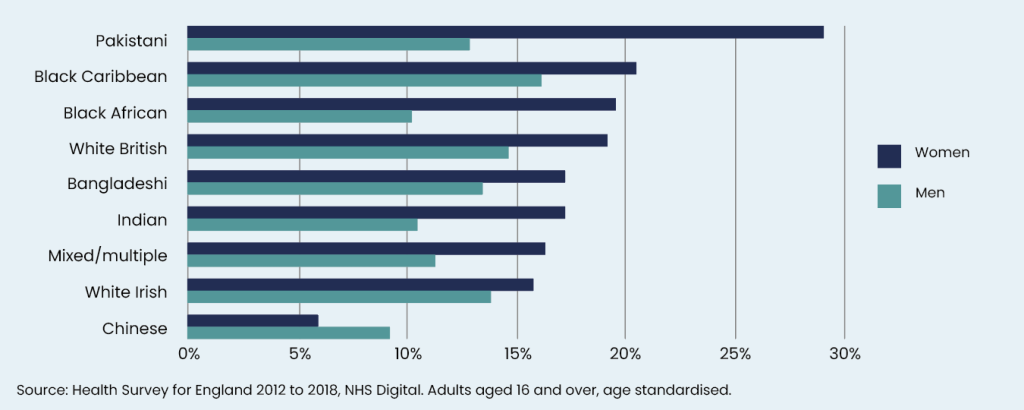
Pakistani (20.8%), and black Caribbean (18.7%) groups were also the most likely to report a long-term MSK condition from Health Survey for England data from 2012 to 2018 (Figure 2) [4]. People living in areas of high deprivation were not only more likely to have an MSK condition but also to develop it at a younger age [5]. Inequalities are compounded through the impact on employment, with MSK conditions being the second commonest reason for economic inactivity behind mental health [6].
The state of chronic pain
Approximately 8 million people in the UK live with chronic pain that is moderately to severely disabling [7], with low back pain being the leading cause of years lived with disability (YLDs) (1). Black people (44% vs 34% for the national average), women (38% vs 30% in men) and those living in the most deprived areas (41% vs 30% in least deprived areas) also suffer from more chronic pain in England [8][9]. Socioeconomic strain and racism have been associated with worse pain outcomes [10][11]. Greater practice list size, rurality, and deprivation have also been associated with high-dose, and perhaps less optimal, opioid prescribing in England [12].
A 2021 report by Versus Arthritis [13] predicted that an integrated care system in England with 3 million people could have 825,000 suffering from chronic pain. The incidence of chronic pain is estimated to grow by 32% in 2040 [14], driven by an ageing population that is living longer with multiple health conditions.
The complex relationship between MSK conditions, mental health and obesity
There is a strong association between mental health and MSK conditions [15]. In the UK, people with an MSK condition are 40% more likely to report a mental health condition [3], possibly due to the conditions being processed through similar biological channels or through MSK-driven disability, loss of work and social isolation [16].
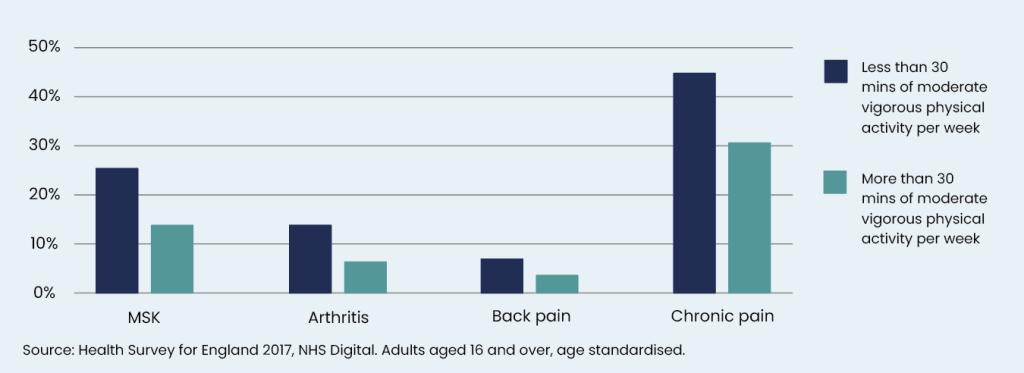
While the interrelation between mental health and MSK conditions is complex and difficult to untangle in terms of cause and effect, they often tend to exist in multimorbidity clusters that are shaped by behavioural factors influenced by one’s environment such as levels of physical activity, smoking and quality of nutrition [16][17]. In fact, lower physical activity is associated with more chronic pain and MSK conditions in England (Figure 3); 35.3% of adults living in the most deprived areas were inactive compared to 16.1% of adults living in the least deprived areas [18].
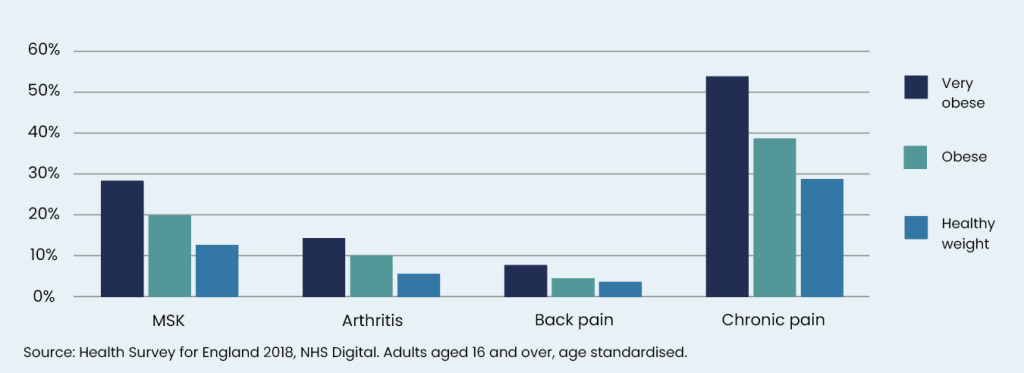
Obesity is also associated with an increased incidence of MSK conditions [19]. Deprived areas have a higher prevalence of people who are overweight (including obesity) compared to the least deprived areas (71.5% vs 59.6%) [18]. People with severe obesity suffer the highest rates of chronic pain, compared to those of a healthy weight (54% vs 29%) (Figure 4) [8]. Obesity is patterned by similar risk factors to MSK and mental health, so addressing those factors using a long-term preventative approach will likely address all of the above conditions [20].
Quality of Care
The 2015 Fair Assessment report by Versus Arthritis found that 1 in 4 statutory assessments of local health needs did not include musculoskeletal conditions, with 62% failing to include back pain [21]. Hip fracture incidence is higher in more deprived areas [5][22], with higher likelihood for delay in surgery due to medical reasons, and higher mortality rates based on a study using the National Hip Fracture Database [22]. Conversely, the 10 Integrated Care Boards with the highest deprivation all had lower rates of hip replacement, despite high prevalences of hip conditions [23]. The Nuffield Trust reported that rates of hip replacement decreased by 9 per 100,000 population in the most deprived decile but increased by 12 per 100,000 population in the least deprived decile (the largest increase of all deciles) between 2008/09 and 2019/20 [24].
The justification for MSK health and care improvement
MSK problems are a key driver of morbidity, but they are also patterned by inequalities with disadvantaged groups consistently reporting a higher prevalence at a younger age and worse quality of care. The consequences of chronic pain and MSK conditions being poorly managed in underserved groups can lead to more poverty, unemployment and worse mental health which compounds the cycle further. Here we review the evidence of what works to improve health and care for people with MSK conditions.
It is also important to note that a significant burden of MSK problems affect working-age populations. We explore this further in our complementary evidence brief What works: Health and care interventions to support people from disadvantaged backgrounds in returning to work [25].
Summary of evidence
We identified 157 relevant studies through EPPI Reviewer, PubMed, Google Scholar and snowballing searching. We prioritised 61 that were the most relevant, robust and up to date. Most studies described inequalities in MSK health and care; there was only limited evidence focused on what works to address these inequalities.
Many studies emphasised the importance of reducing clinical and system barriers to improve the understanding, access and engagement of MSK interventions. Solutions included increasing health literacy, implementation of community-based programmes, integration of MSK services, culturally tailored interventions, and improved services through equity-focused data collection and analysis.
Based on Levesque and colleagues’ work [26], we mapped the evidence to dimensions of care (Figure 5).
Awareness and early intervention
Previous research has found that underserved communities, such as those living in areas of greater deprivation [18] and south Asian communities [27]-[29] do not optimally engage with physical activity due to financial, logistical and cultural barriers. Low health literacy is also associated with worse health outcomes [30]-[32]. While the association is less clear in MSK conditions [33], some studies have revealed that health literacy levels do associate with poorer MSK outcomes, such as with intensity of chronic pain and pain catastrophising (a negative response characterised by exaggerating the pain’s threat), [34]–[36] and self-management [37].
Self-management also requires high self-efficacy, and a review of 60 randomised controlled trials looking at interventions to enhance self-efficacy in people with chronic MSK pain found low-grade evidence for multicomponent exercise and psychological interventions in improving outcomes [38]. However, underserved patients tend to benefit less from self-management interventions due to socioeconomic, cultural, environmental and educational barriers that make adherence challenging [39]–[42]. The structural disadvantage faced by these groups limits self-efficacy and warrants its own research to understand how to best mitigate.
It is unclear if mass media prevention or physical activity campaigns targeted toward minority ethnic populations are more effective [43]. The impact of social media interventions on inequalities is also unclear [44], with low certainty evidence that it may improve physical activity in general but not for underserved groups.
Community-based prevention and physical activity
International reviews have found that community-based interventions to promote physical activity in disadvantaged groups are effective [45][46]. A review of community-based interventions for promoting physical activity found that interventions were more effective if they had a group component and if they were delivered by community organisations (e.g. churches), particularly for socially disadvantaged women [46]. A review of interventions based in rural and remote populations found that community-based education and exercise led to significantly reduced chronic musculoskeletal pain [OR = 1.85 (95% CI 1.22, 2.82)] compared to controls [45]. The authors reported that engaging local staff in the programme delivery, using community locations, and ensuring cultural alignment were important to optimise interventions.
These findings are also supported by UK reviews of physical activity interventions in disadvantaged groups (29,47). Such and colleagues identified 57 physical activity interventions focusing on UK black and minority ethnic groups and found that community capacity-building (i.e. using resources, word-of-mouth, and champions within the community) was an essential element, alongside cultural tailoring [29]. Another review identified barriers to physical activity engagement in people with MSK conditions, which included complex booking procedures, poor translation services, dismissive attitudes to shared decision-making, mistrust, cultural relevance of physical activity, and groups wanting “more than just a sheet of exercises” [47]. Marley and colleagues reviewed the effectiveness of interventions to increase physical activity in adults with persistent MSK pain and found that a higher number of contact hours (more than 8.3 hours) resulted in better outcomes [39].
Improving MSK health literacy
Studies have found that patients often want better education by health professionals, and desire more information about their MSK condition beyond an explanation of its management [37],[40],[41].
Chou and colleagues examined 30 studies to help identify the perceived information needs of patients living with osteoarthritis (OA) and found that they wanted to understand the impact of OA on their quality of life and long-term prognosis, as well as non-pharmacological management [37]. A UK qualitative study by Adams and colleagues found that that information provided by health professionals to patients with MSK problems was not always useful [40]. Both studies found that patients relied on social networks or online communities and emphasised the importance of clear, consistent and accessible (i.e. readily available) communication to better support people with lower health literacy.
Identifying patients at risk of low health literacy is also necessary to address it. A report by the American Orthopaedic Association [41] advocated for the use of the Literacy in MSK Problems (LiMP) questionnaire, a validated instrument for assessing musculoskeletal health literacy via competencies that are integral to making informed decisions regarding MSK health, including anatomical terminology, diagnosis and treatment [48]. However, while its use has been validated in many study settings, there is no evidence to suggest that it is both feasible and effective in real-world clinical settings at improving MSK outcomes.
A review of six studies of MSK education interventions in people with low health literacy found a small, short-term effect on knowledge [49]. The lack of long-term effect may be due to not addressing the underlying barriers and facilitators faced by underserved groups. We know that generally the most effective health literacy interventions tailor information to the cultural and social needs of patients, engage with communities in the real-world setting, use audio visual information and multimedia tools, and focus on upskilling and empowering patients over a sustained period of time [31].
Access and availability
Community integration, self-referral, direct access and digital MSK interventions have been found to improve access; however, evidence is often lacking or mixed in relation to disadvantaged communities. Furthermore, NICE guidelines recommend chronic pain treatments in primary and secondary care that are difficult to access due to cost and availability, like acupuncture and acceptance and commitment therapy (ACT) [50].
Co-location and integration of MSK services
Across all conditions, co-locating and integrating services improves care for underserved groups, but especially for those with co-existing mental health and addiction problems [51].
Crawford and colleagues looked at strategies to increase access to outpatient physiotherapy and found that 7 out of 51 studies evaluated services in unconventional community settings, such as homeless shelters [52]. They found that community located physiotherapy increased patient satisfaction, provided a positive rehabilitation experience, and reduced barriers to accessing care. Berry and colleagues’ UK-based review also found that shifting MSK care to more place-based approaches removed barriers to initial health system engagement [47]. They recommended ‘Community Appointment Days’ which would provide a comprehensive range of MSK support services under one roof, typically in local leisure centres, and offered to patients on MSK referral waiting lists.
A successful example of community integration is the UK-based MSK Hubs programme [53] (see case study box). Developed in partnership with ukactive and several other key stakeholders, the multi-component project created capacity for the delivery of support for MSK health using existing community assets (places and people) in a more affordable and accessible way (both in terms of location and waiting time) [54]. A 2024 evaluation found that 44% of participants reported improvement in the pain management of their condition after attending the programme sessions for 12 weeks [54]. Recommendations for upscaling and successful delivery of the programme included specifying how to engage healthcare professionals and improving referral pathways [54].
Definition: Direct access or self-referral
Patient direct access (also known as self-referral) for MSK care is a system of access in which patients can refer themselves directly to a non-medical first contact professional without having to see anyone else first, or without being told to refer themselves by a medical practitioner [47].
Direct access or self-referral to MSK services
Previous research has found that direct access services for patients with MSK conditions improves outcomes and is more cost-effective than clinician-led care [52],[55]. A review of 26 studies of non-medical triage, self-referral and direct access services for patients with musculoskeletal pain found that, improvements in pain, functional disability and quality of life were consistently similar between direct access patients and GP-led care [55]. Furthermore, evidence shows that direct access patients report less work-related absence due to their MSK conditions compared to GP-led care [55]. A review by Crawford and colleagues found that from 8 out of 51 studies that evaluated health system costs, six had lower costs per episode of care for direct access and two had no cost difference [52].
There is a lack of data examining the impact of self-referral physiotherapy services on inequalities in the UK [56]; however, research from other health services with self-referral pathways show that it is used more by white patients, possibly due to language and literacy barriers [57]. A recent evaluation of patient-initiated follow-up (PIFU) by the NHS Rapid Service Evaluation Team found limited evidence of the impact of PIFU on different patient groups [58]. It is thought that digital exclusion and socioeconomic status influenced engagement with PIFU, although these conclusions are limited by the lack of data collection of demographic characteristics [58]. Babatunde’s review also found that those who used direct access and self-referral services were often younger, slightly more educated and of higher socioeconomic status, suggesting that targeting underserved groups is required [55].
Contrastingly, a recent MSK service evaluation from Sandwell and West Birmingham Trust [59] found that primary care referrals were disproportionately high for the white patient group, while self-referrals were predominantly from black and Asian populations, suggesting the presence of GP access barriers.
From a systems approach perspective, self-referral or direct access use by groups with more health literacy and agency may free up staff capacity and time to support patients with greater needs, though we lack the data to assess if this resource shift happens in practice. Further evidence regarding mitigating inequalities in self-referral can be found in our evidence brief collection [60].
Digital MSK health and care
Digital health interventions (DHIs) such as personal health tracking, web-based programmes, websites and apps have the potential to bridge gaps in access but risk exacerbating inequalities. Hewitt and colleagues reviewed the effectiveness of DHIs for management of MSK conditions and found that, across 19 studies, nine reported statistically significant reductions in pain following digital interventions, and 10 out of 16 studies reporting significant improvements in functional disability [61]. Due to the different digital features within each intervention, it is unclear which components are most effective.
One UK study used expert stakeholder interviews to develop strategies to improve the equity of digital pain management tools [62]. They found that language barriers, learning difficulties such as cognitive impairments or low digital literacy, and lack of comfort with technology negatively impacted use of digital tools. They identified potential strategies across four categories: (a) modifying tools (e.g., zoom functionality for people with visual or dexterity impairments); (b) improving digital skills and physical access to digital resources (e.g., develop easier-to-understand written user instructions about how to complete pain self-reports); (c) improving perceived value of pain self-reports (e.g., materials for healthcare professionals to better interpret pain self-reports); and (d) building trust in technology and research (e.g., enable users to control what information is shared).
Another UK study explored cross-cultural acceptability of digital tools for pain self-reporting and found differences in requirements related to language (e.g. translated in-app instructions, culturally appropriate pain terminologies) and reporting functionality (e.g. pain layers or depth) [63]. They also found differences for pain quality descriptors, such as ‘aching’, ‘gnawing’, and ‘throbbing’, which supports the use of pain assessment using visuals rather than words.
Acceptability and alignment
Tailoring services to meet the cultural needs of underserved patients improves intervention engagement [64]–[68]. Upskilling staff to understand the cultural values and beliefs of their patient population also helps with providing tailored care [69]–[72]. Furthermore, having a workforce that is ethnically diverse and congruent to its target population can ensure acceptability of care given [69][73].
The biopsychosocial framework [74], a theoretical model viewing health and wellbeing more holistically with consideration of influence of social factors, was consistently highlighted in the literature as an important element to MSK care [75]–[78].
Cultural tailoring of interventions
Research suggests that ethnocultural and migration background have significant influence on the pain experience, including coping strategies and therapy engagement [68],[79]–[81]. A review of nine studies looking at the effectiveness of multidisciplinary, activity-based chronic pain interventions for adults of ethnoculturally diverse (ECD) backgrounds found the interventions had poorer outcomes for ECD adults compared to the predominant culture [68]. Concerningly, differences in pain intensity persisted up to three years post-intervention. Another review assessed if multidisciplinary pain interventions were multicultural, and found only 3 of 75 studies included had participants who spoke a nondominant language [79]. A review specifically evaluating chronic pain interventions in recent refugee and immigrant populations found multidisciplinary pain management programs were also effective [80].
A review of 11 studies examining strategies to improve equitable access to early osteoarthritis diagnosis and management for disadvantaged groups found most interventions included education through decision aids or self-management coaching [82]. Interventions were adapted using language translation, frequently visited locations and co-producing with representatives from targeted groups. This is consistent with adaptations suggested in other reviews, with language translation and the use of culturally congruent community champions and venues being the most common [68][80].
A qualitative UK study aiming to explore pain management perceptions and understanding of key components of cognitive behavioural therapy in South Asian community members found that while religious and cultural differences were noted, the more significant differences were noted by age and gender [28]. The authors suggested stratifying pain management interventions by specific age and gender groups as a form of cultural tailoring. They also recommended exercise for pain management be integrated within the context of other meaningful activities which might include walking to the local mosque or spiritual stretching during prayer time.
Cultural tailoring is important for pain management, as evidenced by two case studies [83][84]. A culturally adapted pain management programme based in Bradford, with a large Pakistani community, found statistically significant improvements in anxiety (P<0.01), depression (P<0.01), and self-efficacy (P<0.001) [83]. The pain management intervention included an overview from the hospital’s Muslim chaplain and how Islamic teachings promote self-management, compassion, physical activity and dispelling cultural myths. As literacy is a common problem, audio and video material were presented in Urdu [83]. Though the findings were significant, the programme had a very small sample size (n=6) with no comparison group, so provides more evidence for feasibility rather than clinical or cost-effectiveness.
An Australian feasibility study implemented a cultural mentoring program alongside pain management and physical rehabilitation for chronic musculoskeletal conditions [84], and found higher treatment attendance (75% pre-implementation; 89% post), and high treatment satisfaction (97% pre-implementation; 96% post). Compared to routine care (n = 71), patients receiving mentoring (n = 55) achieved significantly higher Patient Activation Measure scores at 3 months (median change 0 vs 10.3 points, p < 0.01) [84].
Staff training and cultural competency
Mistrust, structural racism and clinician bias can lead to inequalities in MSK health and care. This is particularly true for chronic pain, with several reviews revealing cultural variations in how pain is perceived and subsequently managed [28][67][71][72][85]. A US review examining the psychosocial predictors of chronic MSK pain in black people found that perceived racial or ethnic discrimination in medical providers was associated with worse pain [71]. Different preferences and expectations relating to seeking and receiving pain care, such as practising stoicism and not openly discussing pain with family and community also limited how black people accessed care. Stoicism was also noted in a UK qualitative study that explored the beliefs and lived experiences of British and Punjabi participants with chronic low back pain [72]. They found that Punjabi participants felt a “disruption to their cultural-religious wellbeing” and suffered negative responses and stigma from their wider community, lending itself to stoicism. In both cases, it was unclear whether stoicism had positive or negative impact on pain outcomes though they definitively influenced access and engagement with pain services.
Studies have also shown that South Asians tend to favour passive coping strategies such as massage and rest for chronic pain, rather than active strategies such as exercise which is often prescribed by staff [72][86]. Authors of both reviews suggested strengthening the therapeutic alliance by training providers in cultural humility and having a deeper understanding of the cultural context of pain, aligning management options closer to held beliefs [71][72]. However, the limited evidence of therapeutic alliance in physiotherapy is contrasting. A review by Kinney and colleagues concluded that strong relationships may improve pain outcomes [87], whilst a review by Lakke and Meerman reported that therapeutic alliance did not improve pain outcomes of physical function [88].
A review of seven qualitative studies that explored chronic MSK pain found that healthcare providers’ implicit biases around race, ethnicity, gender, and patients’ unmet expectations negatively influenced the process of care [85]. They described examples where black patients were prescribed fewer medications compared to their white counterparts, and that women were also provided with inadequate pain relief. When patients’ expectations were not met – due to perceived disrespect from providers, or frustration from providers who do not understand reasons behind missed appointments – there were higher dropout rates from pain rehabilitation programs and poorer long-term pain outcomes.
Diverse MSK healthcare workforce
Staff diversity has not only been shown to improve patient outcomes [89], but also patient satisfaction and trust, cultural competence in the patient-provider relationship, health care access for geographically underserved populations, and wider inclusion in research [90][91].
However, there was limited evidence regarding recruitment strategies to improve MSK workforce diversity. A review of 62 studies looking at overcoming barriers to diversity in orthopaedic surgery found implicit biases during the selection process of trainees and negative perceptions of the specialty by potential trainees [73]. The authors suggested trainees required provision of good role models, mentorship and outreach through pipeline programs that target underrepresented students in high school and university.
Notably, studies in non-MSK conditions, predominantly mental health, found that while some participants wanted culturally or ethnically matched staff, others felt it was more important that healthcare professionals were kind, caring and knowledgeable [92], with mixed evidence that ethnic matching of staff is effective [93][94]. It is also important to consider whether underserved individuals would prefer not to be treated by professionals from the community due to concerns about stigma [72][95].
Analysis and Insights
Representative and patient-led MSK data
Poor data can prevent effective action on health inequalities generally. The Ada Lovelace Institute recently published a report describing six “knots” in the data pathway that lead to inequalities: 1) inequalities are poorly understood and measured, 2) there are tensions between local and national priorities for data, 3) data quality varies, 4) data curation can lose the nuance, 5) data poorly reflects the lived experience of patients and communities and 6) limited historical or situational knowledge [96].
A UK review which explored the differential effectiveness of seven MSK interventions as prioritised by Public Health England across disadvantaged groups found that almost all studies lacked an equity focus due to incomplete or missing data relating to ethnicity and socioeconomic characteristics [97]. Another UK review of 10 studies which examined access to secondary and tertiary pain services for minority ethnic groups with chronic pain found that none of the studies specifically assessed ethnic inequalities [98], in part because of a lack of accurate ethnicity coding. In fact, poor ethnicity coding occurs across all health services, limited partly due to patient mistrust and representativeness of ethnic categories with many individuals selecting the “other” category in the absence of alternative choices or free-text fields [99].
There are studies aiming to improve data quality and ethnicity recording, though research in the area is still in its infancy. A recent review to improve data quality relating to health inequalities found evidence for introduction of data collection legislation, senior buy-in, staff training, improved IT infrastructure and data linkage [100]. An unevaluated programme for Cambridgeshire and Peterborough NHS Foundation Trust’s paediatric mental health services developed an interactive, live dashboard to view rates of ethnicity data completion to raise awareness and prompt staff to reflect on the value of data [101].
A UK review also developed a minimum set of MSK indicators for primary care and community services, including three patient-reported outcome measures (PROMs) and one patient-reported experience measures (PREMs) [102]. PROMs and PREMs promote patient-led outcomes; however, PROMs are less likely to be completed by ethnic minority groups and lower socioeconomic groups [103]. A US based study examining the use of hip and knee arthroplasty PROMs in minority ethnic and lower socioeconomic groups recommended translation into different languages, consideration of health literacy, and use of Visual Analog Scales and other pictorial versions [103]. They also suggested more administrative support and resources, surgeon engagement, paper options in addition to digital, e-mail reminders, collecting PROMs prior to the start of the patient visit, information sheets and individually approaching patients [103].
Case study: MSK Hubs Programme
Site selection for the programme was mapped against Indices of Multiple Deprivation (IMD) to ensure delivery to areas experiencing the greatest inequalities, with pilot sites receiving training and support for implementation. Community venue staff and volunteers were upskilled to offer holistic wellbeing service combined with the evidence-based self-management services for arthritis and chronic pain [54]. Service-users were most likely to find out about the MSK Hubs programme through their leisure centre (45.7%), followed by referrals from the GP or physio (18.1%) [54], revealing a demand for individuals to self-refer and to receive support for their condition in a non-clinical setting, in addition to medical referrals.
Limitations
The lack of reviews exploring strategies to address inequalities specifically in MSK health and care limited our conclusions about what interventions were the most effective. However, we were able to draw upon transferable evidence for effective interventions in other health conditions, such as mental health. Most of the included MSK studies lacked an equity-focused analysis by not providing disaggregated data across different characteristics such as ethnicity or socioeconomic status. Chronic pain as an MSK condition was also overly represented in this brief, with conditions such as arthritis, osteoporosis and other rheumatological conditions having less evidence. It is also important to recognise that health and care interventions form only one facet of prevention and treatment of MSK conditions, and optimal MSK health necessitates a cross-sectoral approach targeting multiple social determinants to improve wellbeing and reduce inequalities.
What works: key recommendations
| Recommendation | Target audience | GRADE certainty |
|
Community-based physical activity programmes which are targeted at disadvantaged communities, culturally relevant and held in familiar community settings should be implemented. |
NHS England, ICBs, local authorities and general practices |
⊕ ⊕ ⊕ Moderate |
|
Group activities based in trusted community locations should be implemented, especially targeting women from underserved communities. |
NHS England, ICBs, local authorities and general practices |
⊕ ⊕ Low |
|
MSK programmes, services and communication should be tailored so that the content is easy to understand for people with low health literacy. e.g., by working with patient representatives to ensure written material is understandable and using pictograms, illustrated text, and narrated animations and audio-visual information (in digital material) as much as possible. |
NHS England, ICBs, PCNs, Trusts, pharmacies, and general practices |
⊕ ⊕ ⊕ Moderate |
|
Integrated, community-based physiotherapy services located in underserved communities, particularly unconventional spaces, are likely to improve access and outcomes. |
NHS England, ICBs, PCNs, Trusts, and general practices |
⊕ ⊕ ⊕ Moderate |
|
Self-referral and direct access MSK services without consideration or mitigation for underserved groups may perpetuate inequalities. |
NHS England, ICBs, PCNs, Trusts, and general practices |
⊕ ⊕ Low |
|
Digital health interventions with appropriate modifications addressing differential literacy, linguistic and cognitive needs may improve pain and function outcomes, and are likely to be at least as effective as non-digital activities and should be offered as part of multi-component programmes. |
NHS England, ICBs, PCNs, Trusts, and general practices |
⊕ ⊕ Low |
|
Pain assessment tools should use visual methods wherever possible. |
NHS England, ICBs, PCNs, Trusts, and general practices |
⊕ ⊕ ⊕ Moderate |
|
MSK services should be culturally tailored, including the age and gender of the target population. |
NHS England, ICBs, PCNs, Trusts, and general practices |
⊕ ⊕ ⊕ Moderate |
|
Staff should undergo health equity training that covers cultural competency, anti-stigma and anti-racist training. |
NHS England, ICBs, PCNs, Trusts, and general practices |
⊕ ⊕ Low |
|
The NHS should seek to recruit and retain a diverse workforce in terms of ethnicity, age, educational background and gender, including mentoring programmes. |
NHS England, ICBs, PCNs, Trusts, and general practices |
⊕ ⊕ Low |
|
National and regional teams should provide support and guidance on data collection, including definitions, coding and processing to facilitate standardisation. |
NHS England, ICBs |
⊕ ⊕ Low |
|
Using standardised PROMs and PREMs across the NHS to benchmark MSK services, disseminated in multiple languages and in alternative multimedia formats (e.g. visual scales), may identify areas of unmet need and allow for comparison. |
NHS England, ICBs, PCNs, Trusts, and general practices |
⊕ ⊕ Low |
*GRADE certainty communicates the strength of evidence for each recommendation.
Recommendations which are supported by large trials will be graded highest whereas those arising from small studies or transferable evidence will be graded lower. The grading should not be interpreted as priority for policy implementation – i.e. some recommendations may have a low GRADE rating but likely to make a substantial population impact.
References
- Versus Arthritis. The State of Musculoskeletal Health 2024. Chesterfield, UK: Versus Arthritis; 2024.
- Musculoskeletal health: local profiles – Data | Fingertips | Department of Health and Social Care [Internet]. [cited 2025 Jan 7]
Available from: https://fingertips.phe.org.uk/profile/msk/data#page/1 - GOV.UK [Internet]. [cited 2025 Jan 7]. Musculoskeletal health local profiles: short commentary, January 2024
Available from: https://www.gov.uk/government/statistics/musculoskeletal-health-local-profiles-january-2024-update/musculoskeletal-health-local-profiles-short-commentary-january-2024 - Musculoskeletal health: trends, risk factors and disparities in England [Internet]. [cited 2025 Jan 7].
Available from: https://fingertips.phe.org.uk/static-reports/musculoskeletal-conditions/musculoskeletal-health-trends-risk-factors-and-disparities-in-england.html - Arthritis and Musculoskeletal Alliance (ARMA). Act Now: Musculoskeletal Health Inequalities and Deprivation. 2024;
- Rising ill-health and economic inactivity because of long-term sickness, UK – Office for National Statistics [Internet]. [cited 2025 Jan 21]
Available from: https://www.ons.gov.uk/employmentandlabourmarket/peoplenotinwork/economicinactivity/articles/risingillhealthandeconomicinactivitybecauseoflongtermsicknessuk/2019to2023 - The British Pain Society. UK Pain Messages 2024. 2024.
- Public Health England. Chronic pain in adults 2017: Health Survey for England. 2017;
- Prevalence | Background information | Chronic pain | CKS | NICE [Internet]. [cited 2025 Jan 7].
Available from: https://cks.nice.org.uk/topics/chronic-pain/background-information/prevalence/ - Meints SM, Edwards RR. Evaluating psychosocial contributions to chronic pain outcomes. Chronic Pain Psychiatr Disord. 2018 Dec 20;87:168–82.
- Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019 Aug 1;123(2):e273–83.
- Curtis HJ, Croker R, Walker AJ, Richards GC, Quinlan J, Goldacre B. Opioid prescribing trends and geographical variation in England, 1998–2018: a retrospective database study. Lancet Psychiatry. 2019 Feb 1;6(2):140–50.
- Versus Arthritis. Chronic Pain in England – Unseen, Unequal, Unfair. 2021 Jun.
- REAL Centre. Health in 2040: projected patterns of illness in England. The Health Foundation; 2023 Jul.
- Heikkinen J, Honkanen R, Williams L, Leung J, Rauma P, Quirk S, et al. Depressive disorders, anxiety disorders and subjective mental health in common musculoskeletal diseases: A review. Maturitas. 2019 Sep 1;127:18–25.
- Duffield SJ, Ellis BM, Goodson N, Walker-Bone K, Conaghan PG, Margham T, et al. The contribution of musculoskeletal disorders in multimorbidity: Implications for practice and policy. Ageing Musculoskelet Health. 2017 Apr 1;31(2):129–44.
- Tyrovolas S, Moneta V, Giné Vázquez I, Koyanagi A, Abduljabbar AS, Haro JM. Mental Disorders, Musculoskeletal Disorders and Income-Driven Patterns: Evidence from the Global Burden of Disease Study 2017. J Clin Med. 2020;9(7).
- GOV.UK [Internet]. [cited 2025 Jan 21]. Obesity Profile: short statistical commentary May 2024.
Available from: https://www.gov.uk/government/statistics/update-to-the-obesity-profile-on-fingertips/obesity-profile-short-statistical-commentary-may-2024 - Fortunato LM, Kruk T, Júnior EL. Relationship between obesity and musculoskeletal disorders: systematic review and meta-analysis. Res Soc Dev. 2021 Oct 6;10(13):e119101320212–e119101320212.
- Briggs AM, Woolf AD, Dreinhöfer K, Homb N, Hoy DG, Kopansky-Giles D, et al. Reducing the global burden of musculoskeletal conditions. Bull World Health Organ. 2018 Apr 12;96(5):366–8.
- Arthritis Research UK. A Fair Assessment? Musculoskeletal conditions: The need for local prioritisation. 2015.
- Nisar S, Lamb J, Johansen A, West R, Pandit H. The impact of ethnicity on care and outcome after hip fracture in England and Wales. Bone Jt J. 2024;106-B(10):1182–9.
- Judge A, Javaid MK, Leal J, Hawley S, Drew S, Sheard S, et al. Primary care and hospital care costs for hip fracture patients. In: Models of care for the delivery of secondary fracture prevention after hip fracture: a health service cost, clinical outcomes and cost-effectiveness study within a region of England. Southampton (UK): NIHR Journals Library; 2016.
- Nuffield Trust. Deprivation and access to planned surgery [Internet]. [cited 2025 Jan 21].
Available from: https://www.nuffieldtrust.org.uk/resource/deprivation-and-access-to-planned-surgery - Harasgama S, Lamb D, Kuhn I, Gkiouleka A, Ford J, Wong Y, et al. Evidence Brief: What works – Health and care interventions to support people from disadvantaged backgrounds in returning to work. Health Equity Evidence Centre; 2025.
- Levesque JF, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013 Mar 11;12(1):18.
- Bhatnagar P, Shaw A, Foster C. Generational differences in the physical activity of UK South Asians: a systematic review. Int J Behav Nutr Phys Act. 2015 Jul 19;12(1):96.
- Burton AE, Hissey L, Milgate S. Exploring thoughts about pain and pain management: Interviews with South Asian community members in the UK. Musculoskeletal Care. 2019 Jun 1;17(2):242–52.
- Such E, Salway S, Copeland R, Haake S, Domone S, Mann S. A formative review of physical activity interventions for minority ethnic populations in England. J Public Health Oxf. 2017 Dec 1;39(4):e265–74.
- Ugas M, Mackinnon R, Amadasun S, Escamilla Z, Gill B, Guiliani M, et al. Associations of Health Literacy and Health Outcomes Among Populations with Limited Language Proficiency: A Scoping Review. J Health Care Poor Underserved. 2023;34(2):731–57.
- Harasgama S, Dehn Lunn A, Lamb D, Gkiouleka A, Painter H, Ford J. Evidence brief: What works to improve health and digital literacy in disadvantaged groups. Health Equity Evidence Centre; 2024.
- Nutbeam D, Lloyd JE. Understanding and Responding to Health Literacy as a Social Determinant of Health. Annu Rev Public Health. 2021 Oct 9;42:159–73.
- Loke YK, Hinz I, Wang X, Rowlands G, Scott D, Salter C. Impact of Health Literacy in Patients with Chronic Musculoskeletal Disease–Systematic Review. PLOS ONE. 2012 Jul 6;7(7):e40210.
- Köppen PJ, Dorner TE, Stein KV, Simon J, Crevenna R. Health literacy, pain intensity and pain perception in patients with chronic pain. Wien Klin Wochenschr. 2018 Jan 1;130(1):23–30.
- Kim K, Yang Y, Wang Z, Chen J, Barandouzi ZA, Hong H, et al. A systematic review of the association between health literacy and pain self-management. Patient Educ Couns. 2022 Jun 1;105(6):1427–40.
- Hill CL, Appleton SL, Black J, Hoon E, Rudd RE, Adams RJ, et al. Role of Health Literacy in Self-Reported Musculoskeletal Disorders. Arthritis. 2015 Jan 1;2015(1):607472.
- Chou L, Ellis L, Papandony M, Seneviwickrama KLMD, Cicuttini FM, Sullivan K, et al. Patients’ perceived needs of osteoarthritis health information: A systematic scoping review. PLOS ONE. 2018 Apr 16;13(4):e0195489.
- Martinez-Calderon J, Flores-Cortes M, Morales-Asencio JM, Fernandez-Sanchez M, Luque-Suarez A. Which Interventions Enhance Pain Self-efficacy in People With Chronic Musculoskeletal Pain? A Systematic Review With Meta-analysis of Randomized Controlled Trials, Including Over 12 000 Participants. J Orthop Sports Phys Ther. 2020;50(8):418–30.
- Marley J, Tully MA, Porter-Armstrong A, Bunting B, O’Hanlon J, Atkins L, et al. The effectiveness of interventions aimed at increasing physical activity in adults with persistent musculoskeletal pain: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2017 Nov 22;18(1):482.
- Adams J, Ballinger C, Lowe W, Rowley C, Lueddeke J, Armstrong R, et al. I42 Personal Impact of Lower Levels of Health Literacy on Living with a Musculoskeletal Disease: A Qualitative Interview Study. Rheumatology. 2016 Apr 1;55(suppl_1):i8–9.
- Rosenbaum AJ, Uhl RL, Rankin EA, Mulligan MT. Social and Cultural Barriers: Understanding Musculoskeletal Health Literacy*: AOA Critical Issues. JBJS. 2016;98(7).
- Sheehy-Skeffington J, Rea J. How poverty affects people’s decision-making processes. Joseph Rowntree Foundation: London School of Economics;
- Mosdøl A, Lidal I, Straumann G, Vist G. Targeted mass media interventions promoting healthy behaviours to reduce risk of non‐communicable diseases in adult, ethnic minorities. Cochrane Database Syst Rev. 2017;(2).
- Petkovic J, Duench S, Trawin J, Dewidar O, Pardo Pardo J, Simeon R, et al. Behavioural interventions delivered through interactive social media for health behaviour change, health outcomes, and health equity in the adult population. Cochrane Database Syst Rev. 2021;(5).
- Rajan P, Hiller C, Lin J, Refshauge K, Lincoln M, Leaver A. Community-based interventions for chronic musculoskeletal health conditions in rural and remote populations: A systematic review. Health Soc Care Community. 2021 Nov 1;29(6):1621–31.
- Brand T, Pischke CR, Steenbock B, Schoenbach J, Poettgen S, Samkange-Zeeb F, et al. What Works in Community-Based Interventions Promoting Physical Activity and Healthy Eating? A Review of Reviews. Int J Environ Res Public Health. 2014;11(6):5866–88.
- Berry A, Brady T, Bradley N, Harris N, Flurey C, Niyi-Odumosu F, et al. Supporting People With Musculoskeletal Conditions From Underserved Communities in the United Kingdom to Engage With Physical Activity: A Realist Synthesis and Q-Methodology Study. J Phys Act Health. 2024 Dec 1;21(12):1351–71.
- Rosenbaum AJ, Pauze D, Pauze D, Robak N, Zade R, Mulligan M, et al. Health Literacy in Patients Seeking Orthopaedic Care: Results of the Literacy in Musculoskeletal Problems (LIMP) Project. Iowa Orthop J. 2015;35:187–92.
- Lowe W, Ballinger C, Protheroe J, Lueddeke J, Nutbeam D, Armstrong R, et al. Effectiveness of Musculoskeletal Education Interventions in People With Low Literacy Levels: A Systematic Review. Arthritis Care Res. 2013 Dec 1;65(12):1976–85.
- Rationale and impact | Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain | Guidance | NICE [Internet]. NICE; 2021 [cited 2025 Mar 4].
Available from: https://www.nice.org.uk/guidance/ng193/chapter/Rationale-and-impact#acupuncture-for-chronic-primary-pain-2 - Richardson A, Richard L, Gunter K, Cunningham R, Hamer H, Lockett H, et al. A systematic scoping review of interventions to integrate physical and mental healthcare for people with serious mental illness and substance use disorders. J Psychiatr Res. 2020 Sep 1;128:52–67.
- Crawford T, Parsons J, Webber S, Fricke M, Thille P. Strategies to Increase Access to Outpatient Physiotherapy Services: A Scoping Review. Physiother Can. 2022 May 1;74(2):197–207.
- MSK Hubs Programme [Internet]. ukactive. [cited 2025 Jan 23].
Available from: https://www.ukactive.com/projects/msk-hubs/ - ukactive. Transforming gyms into community musculoskeletal (MSK) Hubs: Mobilising the UK leisure sector to deliver inclusive, accessible, personalised and gamified health services for older adults with MSK conditions. 2024.
- Babatunde OO, Bishop A, Cottrell E, Jordan JL, Corp N, Humphries K, et al. A systematic review and evidence synthesis of non-medical triage, self-referral and direct access services for patients with musculoskeletal pain. PLOS ONE. 2020 Jul 6;15(7):e0235364.
- FCP phase 3 evaluation data | The Chartered Society of Physiotherapy [Internet]. 2020 [cited 2025 Jan 24].
Available from: https://www.csp.org.uk/professional-clinical/improvement-innovation/first-contact-physiotherapy/fcp-phase-3-evaluation - Harwood H, Rhead R, Chui Z, Bakolis I, Connor L, Gazard B, et al. Variations by ethnicity in referral and treatment pathways for IAPT service users in South London. Psychol Med. 2021/08/02 ed. 2023;53(3):1084–95.
- Sherlaw-Johnson C, Georghiou T, Reed S, Hutchings R, Appleby J, Bagri S. Investigating innovations in outpatient services: a mixed-methods rapid evaluation. Chapter 3 Evaluation of Patient-Initiated Follow-Up. Health Soc Care Deliv Res. 2024;12(38).
- Shah W, Newham R, Casey C, Burgess R. Clinical Characteristics and Variation in Musculoskeletal Complexity of Different Ethnic Populations Accessing Sandwell and West Birmingham Hospital’s MSK Service: A Service Evaluation. Musculoskeletal Care. 2024 Dec 1;22(4):e70012.
- Harvey-Sullivan A, Lynch H, Ford J. Evidence Brief: What works – Mitigating inequalities in patient self-referral to specialist services. Health Equity Evidence Centre; 2024.
- Hewitt S, Sephton R, Yeowell G. The Effectiveness of Digital Health Interventions in the Management of Musculoskeletal Conditions: Systematic Literature Review. J Med Internet Res. 2020 Jun 5;22(6):e15617.
- Ali SM, Gambin A, Chadwick H, Dixon WG, Crawford A, Van der Veer SN. Strategies to optimise the health equity impact of digital pain self-reporting tools: a series of multi-stakeholder focus groups. Int J Equity Health. 2024 Nov 11;23(1):233.
- Ali SM, Lee RR, McBeth J, James B, McAlister S, Chiarotto A, et al. Exploring the Cross-cultural Acceptability of Digital Tools for Pain Self-reporting: Qualitative Study. JMIR Hum Factors. 2023 Feb 8;10:e42177.
- Gkiouleka A, Harasgama S, Pearce H, Kuhn I, Dehn Lunn A, Torabi P, et al. What works: Improving access, uptake and optimisation of behavioural interventions in the health care setting to better meet the needs of disadvantaged groups. Health Equity Evidence Centre; 2024.
- Wang E, Rodrigues IB, Li LC. Effectiveness of Tailored Self-Management Interventions for People with Chronic Musculoskeletal Conditions: a Systematic Review and Meta-Analysis. Physiother Can. 2024 May 31;e20230050.
- Gagliardi AR, Abbaticchio A, Theodorlis M, Marshall D, MacKay C, Borkhoff CM, et al. Multi-level strategies to improve equitable timely person-centred osteoarthritis care for diverse women: qualitative interviews with women and healthcare professionals. Int J Equity Health. 2023 Oct 7;22(1):207.
- Arthur L, Rolan P. A systematic review of western medicine’s understanding of pain experience, expression, assessment, and management for Australian Aboriginal and Torres Strait Islander Peoples. PAIN Rep. 2019;4(6).
- Mojdehi S, Brady B, Tang C, Peiris CL. The effectiveness of multidisciplinary, activity-based chronic pain interventions for adults of ethnoculturally diverse backgrounds: a systematic review with meta-analysis. Disabil Rehabil. 2025 Jan 16;47(2):314–23.
- Ford J, Harasgama S, Lamb D, Dehn Lunn A, Gajria C, Painter H, et al. Evidence Brief: What works: Empowering health care staff to address health inequalities. Health Equity Evidence Centre; 2024.
- Calikyan A, Silverberg J, McLeod KM. Osteoporosis Screening Disparities among Ethnic and Racial Minorities: A Systematic Review. J Osteoporos. 2023 Jan 1;2023(1):1277319.
- Bakhshaie J, Penn TM, Doorley J, Pham TV, Greenberg J, Bannon S, et al. Psychosocial Predictors of Chronic Musculoskeletal Pain Outcomes and their Contextual Determinants Among Black Individuals: A Narrative Review. J Pain. 2022 Oct 1;23(10):1697–711.
- Singh G, Newton C, O’Sullivan K, Soundy A, Heneghan NR. Exploring the lived experience and chronic low back pain beliefs of English-speaking Punjabi and white British people: a qualitative study within the NHS. BMJ Open. 2018 Feb 1;8(2):e020108.
- Rama E, Ekhtiari S, Thevendran G, Green J, Weber K, Khanduja V. Overcoming the Barriers to Diversity in Orthopaedic Surgery: A Global Perspective. JBJS. 2023;105(23).
- Engel GL. The Need for a New Medical Model: A Challenge for Biomedicine. Science. 1977 Apr 8;196(4286):129–36.
- van Erp RMA, Huijnen IPJ, Jakobs MLG, Kleijnen J, Smeets R. Effectiveness of Primary Care Interventions Using a Biopsychosocial Approach in Chronic Low Back Pain: A Systematic Review. Pain Pr. 20181202nd ed. 2019 Feb;19(2):224–41.
- Holopainen R, Simpson P, Piirainen A, Karppinen J, Schütze R, Smith A, et al. Physiotherapists’ perceptions of learning and implementing a biopsychosocial intervention to treat musculoskeletal pain conditions: a systematic review and metasynthesis of qualitative studies. PAIN. 2020;161(6).
- Hochheim M, Ramm P, Amelung V. The effectiveness of low-dosed outpatient biopsychosocial interventions compared to active physical interventions on pain and disability in adults with nonspecific chronic low back pain: A systematic review with meta-analysis. Pain Pract. 2023 Apr 1;23(4):409–36.
- Kamper SJ, Apeldoorn AT, Chiarotto A, Smeets RJ, Ostelo R, Guzman J, et al. Multidisciplinary biopsychosocial rehabilitation for chronic low back pain. Cochrane Database Syst Rev. 2014;(9).
- Brady B, Veljanova I, Chipchase L. Are multidisciplinary interventions multicultural? A topical review of the pain literature as it relates to culturally diverse patient groups. PAIN. 2016;157(2).
- Altun A, Brown H, Sturgiss L, Russell G. Evaluating chronic pain interventions in recent refugees and immigrant populations: A systematic review. Patient Educ Couns. 2022 May 1;105(5):1152–69.
- Hussain R, Bhatti-Ali R. The effectiveness of culturally adapted pain management programmes for south Asian populations. Health Psychol Update. 2021 Sep 1;30:26–31.
- Borkhoff CM, Wieland ML, Myasoedova E, Ahmad Z, Welch V, Hawker GA, et al. Reaching those most in need: A scoping review of interventions to improve health care quality for disadvantaged populations with osteoarthritis. Arthritis Care Res. 2011 Jan 1;63(1):39–52.
- Shoiab M, Sherlock R, Bhatti Ali R, Suleman A, Arshad M. A language specific and culturally adapted pain management programme. Physiotherapy. 2016 Nov 1;102:e197–8.
- Brady B, Sidhu B, Jennings M, Boland R, Hassett G, Chipchase L, et al. The feasibility of implementing a cultural mentoring program alongside pain management and physical rehabilitation for chronic musculoskeletal conditions: results of a controlled before-and-after pilot study. BMC Musculoskelet Disord. 2023 Jan 19;24(1):47.
- Emerson AJ, Oxendine RH, Chandler LE, Huff CM, Harris GM, Baxter GD, et al. Patient and Provider Attitudes, Beliefs, and Biases That Contribute to a Marginalized Process of Care and Outcomes in Chronic Musculoskeletal Pain: A Systematic Review—Part I: Clinical Care. Pain Med. 2022 Apr 1;23(4):655–68.
- Rogers A, Allison T. What if my back breaks?: Making sense of musculoskeletal pain among South Asian and African–Caribbean people in the North West of England. J Psychosom Res. 2004 Jul 1;57(1):79–87.
- Kinney M, Seider J, Beaty AF, Coughlin K, Dyal M, Clewley D. The impact of therapeutic alliance in physical therapy for chronic musculoskeletal pain: A systematic review of the literature. Physiother Theory Pract. 2020 Aug 2;36(8):886–98.
- Lakke SE, Meerman S. Does working alliance have an influence on pain and physical functioning in patients with chronic musculoskeletal pain; a systematic review. J Compassionate Health Care. 2016;3:1–10.
- Gomez LE, Bernet P. Diversity improves performance and outcomes. J Natl Med Assoc. 2019 Aug 1;111(4):383–92.
- LaVeist TA, Pierre G. Integrating the 3Ds—Social Determinants, Health Disparities, and Health-Care Workforce Diversity. Public Health Reports®. 2014 Jan 1;129(1_suppl2):9–14.
- Yelton MJ, Jildeh TR. Cultural Competence and the Postoperative Experience: Pain Control and Rehabilitation. Arthrosc Sports Med Rehabil. 2023 Aug 1;5(4):100733.
- Mir G, Meer S, Cottrell D, McMillan D, House A, Kanter JW. Adapted behavioural activation for the treatment of depression in Muslims. J Affect Disord. 2015 Jul 15;180:190–9.
- Hall GCN, Ibaraki AY, Huang ER, Marti CN, Stice E. A Meta-Analysis of Cultural Adaptations of Psychological Interventions. Spec 50th Anniv Issue Honor Past Look Future Updat Semin Behav Ther Publ Curr Ther Future Dir Part II. 2016 Nov 1;47(6):993–1014.
- Swift JK, Callahan JL, Cooper M, Parkin SR. The impact of accommodating client preference in psychotherapy: A meta-analysis. J Clin Psychol. 2018 Nov 1;74(11):1924–37.
- McEvoy P, Williamson T, Kada R, Frazer D, Dhliwayo C, Gask L. Improving access to mental health care in an Orthodox Jewish community: a critical reflection upon the accommodation of otherness. BMC Health Serv Res. 2017 Aug 14;17(1):557.
- Ada Lovelace Institute. A knotted pipeline: data-driven systems and inequalities in health and social care. 2022 Nov.
- Peat G, Jordan KP, Wilkie R, Corp N, van der Windt DA, Yu D, et al. Do recommended interventions widen or narrow inequalities in musculoskeletal health? An equity-focussed systematic review of differential effectiveness. J Public Health. 2022 Sep 1;44(3):e376–87.
- Leach E, Ndosi M, Jones GT, Ambler H, Park S, Lewis JS. Access to Chronic Pain Services for Adults from Minority Ethnic Groups in the United Kingdom (UK): a Scoping Review. J Racial Ethn Health Disparities. 2024 Dec 1;11(6):3498–508.
- Bignall T, Phillips J. Improving the recording of ethnicity in health datasets: Exploring the views of community respondents and the healthcare workforce. Wellcome Trust: Race Equality Foundation; 2022 Nov.
- Moorthie S, Peacey V, Evans S, Phillips V, Roman-Urrestarazu A, Brayne C, et al. A Scoping Review of Approaches to Improving Quality of Data Relating to Health Inequalities. Int J Env Res Public Health. 2022 Nov 29;19(23).
- Goodman JR, Karamat A, Evans S, Lafortune L. Case study: How health and care systems can improve ethnicity data collection to help combat inequality. Wellcome Trust; 2024 Oct.
- Burgess R, Lewis M, Hill JC. Benchmarking community/primary care musculoskeletal services: A narrative review and recommendation. Musculoskeletal Care. 2023 Mar 1;21(1):148–58.
- Konopka JA, Bloom DA, Lawrence KW, Oeding JF, Schwarzkopf R, Lajam CM. Non-English Speakers and Socioeconomic Minorities are Significantly Less Likely to Complete Patient-Reported Outcome Measures for Total Hip and Knee Arthroplasty: Analysis of 16,119 Cases. Proc 2022 AAHKS Annu Meet. 2023 Jul 1;38(7, Supplement 2):S69–77.