What works: Payment mechanisms to improve prevention spending in health care settings

We have decades of evidence on the clinical and cost-effectiveness of investing in prevention. However, current health and care funding mechanisms do not facilitate investment in prevention. Here we explore what works best to increase and improve funding for prevention defined as any healthcare-based initiative that enhances long-term patient outcomes by reducing harmful exposure, disease onset, and illness progression across all life stages.
What works- Payment mechanisms[PDF 254kb]
Download documentSummary
We have decades of evidence on the clinical and cost-effectiveness of investing in prevention. However, current health and care funding mechanisms do not facilitate investment in prevention. Here we explore what works best to increase and improve funding for prevention.
Based on Health Equity Evidence Centre living evidence maps, a Medline search for review studies and snowball searching, we identified and reviewed 51 studies and grey literature reports. We found evidence to support the following:
- Investing in prevention reduces future costs and is extremely cost effective. The benefits on mortality are mostly realised over the course of 4–5 years, and almost completely realised by 8 years.
- Using capitation payments incentivise long-term, complex interventions.
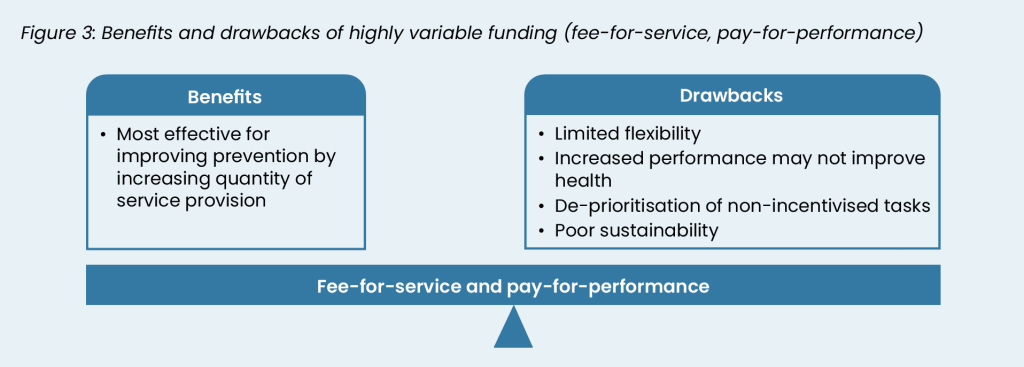
- Using fee-for-service and pay-for-performance payments incentivise shorter-term, specific preventative interventions. These need to be balanced against drawbacks, which include limited flexibility, de-prioritisation of other tasks, and poor sustainability.
- Considering equity in any funding model and allocating resources proportionate to need to improve health outcomes.
There are several other funding mechanisms which do not have enough evidence to understand their likely impact, such as Social Impact Bonds, Prevention Standards, National Prevention Funds, Prevention Departmental Expenditure Limits and reducing existing discount rates. Several return on investment tools exist to help local health and care commissioners understand the long-term impact, but we did not find any studies examining the impact of their implementation.
Current challenges
Investment in prevention is linked to improved health outcomes [1][2][3][4][5][6][7]. One example is Public Health investment. In the UK, local authority public health expenditure is three to four times more cost effective than healthcare expenditure [2]. In England, a 1% increase in public health expenditure was associated with an estimated 0.15% decrease in prevalence of multimorbidity between 2013-2019 [8]. The positive outcomes of preventative interventions take time. Previous research has suggested that most benefits of public health investment are realised within four to five years, while almost all benefits are realised after eight years [1]. Investing in prevention is important if health systems aim to manage long-term capacity and demand by “compressing morbidity” until later life. The Compression of Morbidity Theory proposes that early interventions in midlife delay the onset of ill health until relatively later in life, reducing the overall burden of illness [9].
What is prevention?
Prevention is a nebulous concept. Here we use it to mean any healthcare-based initiative that enhances long-term patient outcomes by reducing harmful exposure, disease onset, and illness progression across all life stages. This includes health care action on lifestyle factors, such as smoking, obesity and physical activity, and clinical interventions to reduce the impact of modifiable risk factors, such as hypertension case finding, diabetes prevention programmes and health checks.
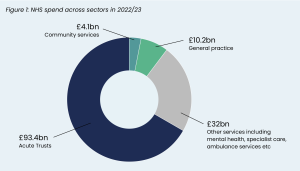
Despite the benefits of prevention, the funding structure of the NHS is currently poorly set up to invest and incentivise preventative health. The Darzi review highlighted funding imbalances in the NHS. Continual pressure to allocate more resources into acute services have resulted in acute trusts receiving the vast majority of NHS spending while Primary and Community Care, where more prevention initiatives occur, receive much less (Figure 1). Local authority public health expenditure was cut in real terms by 28% per person between 2015/16 and 2023/24 [10].
The three most common reimbursement mechanisms are capitation, fee-for-service (FFS) and pay-for-performance (P4P) [11]. These are described in the table on page 3. Other mechanisms do exist but are used less. For example, in some countries, there is reduced private ownership and GPs are paid a set salary.
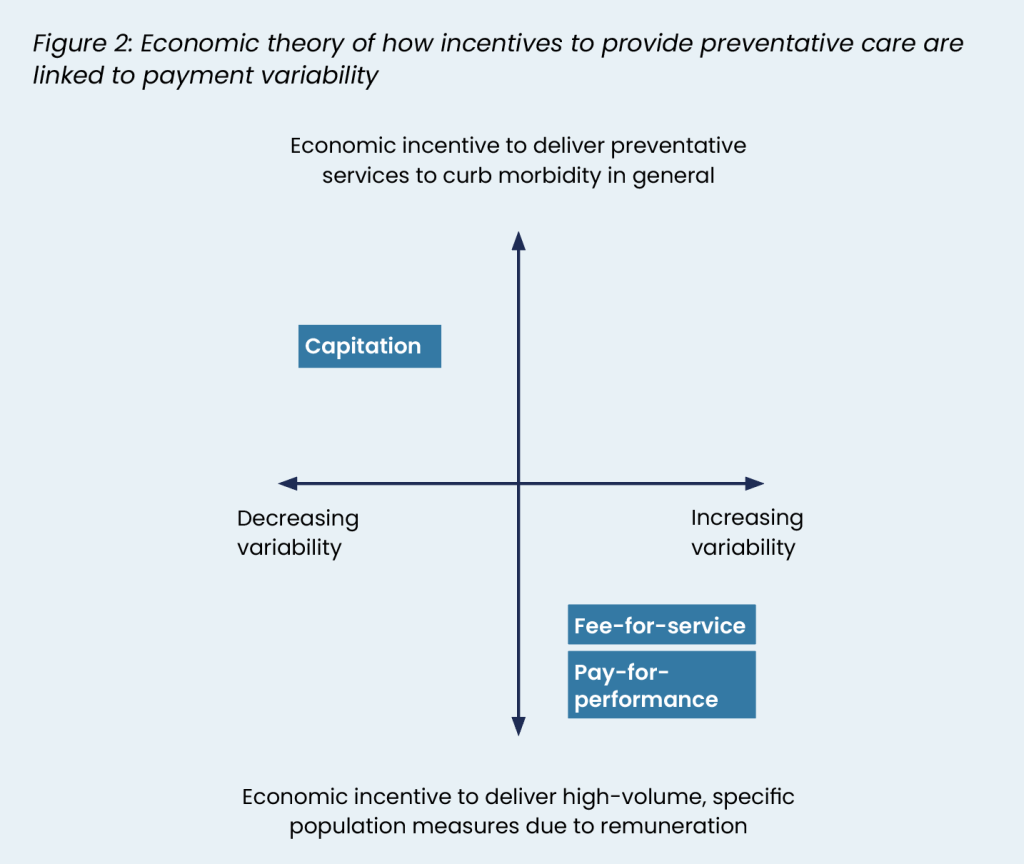
Based on economic theory, a payment mechanism’s incentive to provide long-term preventative care depends on its variability, i.e. the degree to which payments vary based on activity. Generally, as payment variability increases, incentive to provide long-term preventive care diminishes [12].
In more variable payment mechanisms, like FFS or P4P, providers are only financially motivated to deliver preventive care if specific reimbursements are available for those services. The focus centres on meeting thresholds for financial reimbursement rather than long-term outcomes. Conversely, less variable reimbursement models, such as capitation, encourage providers to focus on prevention to reduce their own long-term costs (see Figure 2).
The Darzi Review highlights the need for improved long-term population health, reduced health care costs and improved productivity. Effective prevention achieves all of these, however increasing funding is essential to leverage its potential to do so. Here we review the evidence of what works in a health care setting to improve long-term funding for prevention. This includes previously used payment mechanisms and more novel models. We have not included financial interventions targeted at individuals, such as financial incentives to stop smoking, direct cash transfers, establishment of universal medical savings accounts or cost-sharing models.
| Payment mechanism | Description | Example |
| Capitation | Health care organisations are paid a fixed fee per patient, regardless of the services used. | Global sum that a general practice is paid annually per weighted patient on their list. |
| Fee-for-service (FFS) | Organisations are reimbursed for each unit of care that they deliver. | A hospital performing a flexible sigmoidoscopy to screen for colorectal cancer and being reimbursed the set national tariff. |
| Pay-for-performance (P4P) | Organisations are paid based on quality of provision of care, as measured by specific indicators. | Quality and Outcomes Framework (QOF) reimburses general practices in England based on achievement against standards of clinical processes, prescribing, and patient outcomes. Performance measures constitute a wide variety of prevention-based activities. The total cost to the NHS in 2022-2023 was over £768 million. |
Summary of evidence
The evidence on prevention spending was primarily linked to immunisation, screening, and medical management. Research focused on broader prevention was limited, although translational research highlighted several key points. Overall, literature identified funding as an important factor in prevention. Evidence focused on:
- Traditional funding models, such as capitation, fee-for-service and pay-for-performance.
- Less traditional models, such as non-payment and social impact bonds.
- Tools to support local decision makers, such as return on investment tools.
- Proposed funding models described in the literature which lack evaluation or evidence.
Capitation
Models with lower payment variability, such as capitation, are better at incentivising more complex and longer-term prevention [6]. For example, a Canadian study reported that patients in capitation plans were more likely than patients in an FFS plan to have diabetes monitoring and three types of cancer screening. Over ten years, there was greater improvement in diabetes and cervical cancer screening for patients in capitation plans [13]. A second found that compared to patients in an FFS plan, patients in a plan that blended capitation and FFS had improved performance for diabetes and obesity prevention. They were also more likely to receive smoking cessation support [14]. A US study found that general practitioners whose reimbursement consisted of more than 75% capitation, as opposed to FFS, were three times more likely to provide patient education [15].
The impact of switching from FFS or P4P to capitation may lead to different outcomes for different conditions. This is likely as increased flexibility and decreased financial pressure allowed physicians to change priorities. A study investigating the effect of this in the US on cancer screening found a range of outcomes for different forms of cancer without a clearly identified pattern [16].
We did not find any evidence that explored factors that influence the effectiveness of capitation plans in encouraging prevention.
One drawback of capitation is that it is only successful when sufficiently funded. When funding is restricted, funding priority is shifted to acute, reactive forms of care, rather than long-term prevention. This results in the loss of capitation’s benefits, as long-term reductions of clinical need are not sufficiently incentivised compared to more pressing, short-term clinical needs.
Fee-for-service and pay-for-performance
When aiming to improve prevention through increasing the quantity of a specific service, highly variable funding, such as FFS and P4P are better than less variable funding sources such as capitation [6][7].
For both P4P and FFS, the most convincing evidence examines vaccination [6][7]. Two systematic reviews, one with meta-analysis, reported increased vaccination rates following the introduction of P4P programs [6][7]. Amalgamated findings from the same reviews reported that FFS models increased immunisation rates [6][7]. Stronger evidence was found for higher FFS payments, compared to the impact of FFS alone.
In a Cochrane review, pay-for-performance increased childhood immunisation status by 27% compared to capitation or salaried models and increased guideline-driven prescribing of anti-hypertensives by 7%. The only key factors identified for success were the balance between size of funding versus effort required [6].
The specific effects of FFS and P4P on screening were unclear due to small numbers of studies predominantly from the US and a wide range of different screening programmes. One systematic review suggested that P4P schemes could improve screening rates. However, results were more substantial when P4P schemes were targeted at individual physicians (a 60% to 145% increase in screening rates) rather than practices (2.4% to 11.0% increase), making it less useful in the UK context [16]. Specifically for cancer screening, most studies showed limited or no effects of financial incentives on breast and cervical cancer screening, with some positive or partial effects for colorectal cancer screening [17]. Similarly, evidence for FFS was limited. Of the three studies investigating the impact of increased FFS payments on screening rates, two found that higher reimbursement rates were associated with increased screening, while one study found no link between increased payments and improved cancer screening rates [16]. A UK study of the Quality Outcomes Framework (QOF) and cervical screening found a decline in screening rates from 2013/14 to 2021/22 (77% to 72%), lower than the 80% threshold of screening level set as the QOF standard [18].
Evidence from the QOF has formed much of the evidence base regarding P4P, especially in the English context. The QOF is the predominant P4P scheme in general practice and reimburses general practices by performance against 76 indicators mostly measuring preventative care quality. While original evidence was positive [19][20], revised and more detailed analysis is more mixed. In many cases, positive trends in preventive care had begun before the QOF implementation, and post-intervention results did not consistently show sustained improvements [21][22][23]. Additionally, the impact on long-term health is limited, with findings suggesting that the QOF was not associated with reductions in mortality [24].
Evidence is insufficient to reliably comment on the difference between FFS and P4P. Only one study compared FFS with P4P, finding that a P4P scheme combined with capitation, which rewarded achieving 60% or 80% cancer screening rates, was more effective than a system combining FFS with capitation [6].
Potential drawbacks of FFS and P4P described in the literature include:
- Both FFS and P4P models tend to confine care delivery to predefined standards, limiting the flexibility required for certain types of preventive care [6].
- Achieving P4P targets does not always correlate with improved health outcomes [23][25][26].
- FFS and P4P payments may lead to prioritisation of incentivised tasks over other important but non-incentivised preventive measures [26]. For example, performance in managing conditions outside the QOF worsened since its introduction [22][27].
- FFS and P4P funding may only improve outcomes in the time that it is in use, and not drive long-term changes [6][7]. For example, the QOF is no longer used in Scotland, following the government labelling it as outdated and over-bureaucratic [28]. This was associated with a decrease in measured performance in 75% of indicators that practices were previously reimbursed for [28]. While this may suggest support of continuing such a scheme, it raises issues regarding its sustainability: if performance worsens whenever an indicator is removed, it suggests the QOF is not effective in changing practice long term when additional payments are removed in the presence of competing resource pressures [29].
Non-payment
Non-payment, rather than financial rewards, can be used to reduce rates of adverse medical outcomes. A Cochrane review examined evidence on this, identifying US schemes that penalised hospitals for not meeting quality targets for surgical site infections, catheter-associated infections, antimicrobial use, hospital-acquired pressure ulcers, and inpatient falls [30]. These led to a reduction in adverse clinical events. The impact was larger compared with studies evaluating financial rewards for good performance. Another study, investigating surgical quality more generally rather than prevention, supported these findings: results suggested that a P4P programme with a penalty design could be more effective than programmes using rewards, or a combination of rewards and penalties [31].
Social impact bonds
Social impact bonds (SIBs) are a financing mechanism whereby private investors fund preventative programmes upfront. These are closely linked with ‘outcome-based contracts’ where the government or other organisations repay investors only if the programme achieves predefined outcomes. Whether repayment occurs can be totally or partially based on whether the target outcome was achieved [32]. In theory, this shifts the risk away from the public sector, with any payments being made upon successful achievement of predefined outcomes [33].
Global evidence investigated the use of 11 SIBs for non-communicable disease worldwide conducted in New Zealand, Canada, the United Kingdom, the USA, Japan, Israel, Australia and the Netherlands [34]. These all used a non-medical intervention focused on prevention including patient education, social prescribing, residential care, screening and exercise. Three from the UK were identified. One case study is detailed in Box 3. Overall, findings were limited by a small sample size. Of the four completed SIBs, three met all targets with two exceeding these, while one met some of the targets. Of the SIBs ongoing at the time of the review, two were partially meeting targets, one was below targets and four had not disclosed performance. Common factors of the SIBs meeting target outcomes were evidence-based interventions, multiple service providers and the use of an intermediary between contractor and supplier.
Social impact bond example: Newcastle’s Way to Wellness Scheme
In Newcastle a social impact bond project initiating a community based social prescribing scheme was set up in 2015. The seven-year project required private sector investment from Bridges Ventures of £1.6m. Its targets were to 1) improve self-management of long-term conditions by an average of 1.4 points, and 2) reduce secondary care and acute costs by 22%. If this wasn’t achieved, the payout was undisclosed, but it was documented that all investment could be lost, while if targets were achieved payout would be 1.38 times initial investment. These targets were exceeded: well-being star scores improved by an average 3.4 points and there was an estimated 45% reduction in hospital costs for patients. The Cabinet Office Social Outcomes Group and the local Clinical Commissioning Group funded the project.
A 2013 article proposed seven factors required for an SIB to be successful for preventative care based on the experience in Australia [32]. Key facilitators included: 1) preventative in nature, 2) targeting an area of high social need, 3) evidence-based, 4) directly measurable, 5) aligned to incentives of government (e.g. would lower costs should it be successful), 6) savings greater than costs if successful and 7) government appetite for SIBs. Potential drawbacks of SIB described in the literature include:
- Cost of negotiating an SIB may outweigh the savings [34].
- Evaluations describe the practice of ‘cream-skimming’ i.e. private investors selecting interventions that are most easily achieved [34].
- Reliance on performance-based outcomes may lead to gamesmanship [35].
- Potential marketisation of the public or disadvantaged groups which may change the relationship between health care and the public [36].
Tools to support investment in prevention
Return on investment (ROI) tools quantify resource and financial consequences of implementing interventions nationally and locally and help the most cost-effective interventions to be identified. Several publicly available ROI tools exist, including those for musculoskeletal disease, sexual and reproductive health and colorectal cancer [37][38][39]. Efficiency of current spending can also be detected. For example, the Spending and Outcomes Tool (SPOT) allows commissioners to compare spending and outcome measures against other local authorities. This allows identification of programmes with outcomes that differ from similar authorities, prompting further investigation [40]. We did not find any studies which measure the impact of implementing ROI or SPOT tools in local decision making.
Other funding models which may be effective but lack evidence
A grey literature search identified several reports proposing ways to increase prevention spending. We did not find evidence, either positive or negative, regarding their likely outcome. They include:
- The Hewitt Review recommended increasing the share of Integrated Care Systems’ (ICS) budgets dedicated to prevention by 1% over five years, committing to a Prevention Standard [41]. Alternatively, a prevention standard could increase budget allocation for prevention proportionately by financial metrics, such as GDP or NHS spending.
- Demos, supported by the Health Foundation, proposed creating a Preventative Departmental Expenditure Limit [42]. Currently, government departments are allocated separate Capital Departmental Expenditure Limits (CDEL) and Resource Departmental Expenditure Limits (RDEL) primarily to ensure that there is long-term investment in public services capital spending rather than focusing on short-term issues. A Preventative Departmental Expenditure Limits would operate in the same way to ensure that government departments had dedicated budgets to invest in long-term prevention.
- Both the IPPR and the Faculty of Public Health advocated for a national ring-fenced prevention fund which would fund local initiatives above and beyond existing health care and public health programmes [43][44].
- One mechanism recommended by Demos, and elsewhere, is to alter existing discount rates. Discount rates adjust the expected costs and benefits of an intervention by accounting for when they are likely to be achieved. NICE currently uses a 3.5% discount rate, meaning that future benefits are reduced by 3.5% every year. For example, one year of good health has 30% less weighting in economic models after 10 years compared to the first year, or a cost saving of £100 after 10 years is only valued at £70. Discounting is used because the public value immediate health benefits more than future health benefits, and to account for the cost of borrowing [45]. Larger discount rates reduce the value of long-term intervention benefits. Lowering these rates would support a greater focus on long-term preventive measures.
Further considerations
Having an equity focus leads to more efficient and equitable health care outcomes. For instance, when NHS funding was increased and adjusted for clinical need in 2002, there was a notable reduction in overall mortality and mortality inequalities. These improvements were driven by improvements in areas with higher levels of deprivation [46]. Adjusting general practice funding based on deprivation data could enhance funding efficiency, with the most significant impact by adjusting non-capitation funding streams [47].
What works: Key recommendations
| Recommendation | Target audience | GRADE certainty |
| Spending on prevention is cost-effective and efficient in improving population health and should be increased. | NHS England, DHSC, ICBs and local authorities | ⊕ ⊕ ⊕ ⊕
High |
| Less variable funding (e.g., capitation) should be considered when funding longer-term, more complex forms of prevention, and when organisational flexibility is more important. | NHS England, DHSC and ICBs | ⊕ ⊕ ⊕
Moderate |
| More variable funding mechanisms (e.g., pay-for-performance, fee-for-service) should be considered for situations when simply an increase in the quantity of preventative care is required, especially for vaccination. | NHS England, DHSC and ICBs | ⊕ ⊕ ⊕
Moderate |
| Pay-for-performance incentives should focus on improving adherence to guidelines. | NHS England, DHSC and ICBs | ⊕ ⊕
Low |
| The use of fee-for-service and pay-for-performance funding mechanisms should be balanced against their drawbacks, including limited flexibility, uncertainty of impact on health outcomes, de-prioritisation of other activities and poor sustainability if withdrawn. | NHS England, DHSC and ICBs | ⊕ ⊕ ⊕
Moderate |
| Reducing discount rates used in cost-benefit analysis should be considered to increase value placed on long-term outcomes. | NHS England, DHSC and ICBs | ⊕ ⊕
Low |
| Consider strategic use of social impact bonds to increase preventive funding and innovation. | NHS England, DHSC and ICBs | ⊕ ⊕
Low |
| Consider prevention standards as a mechanism for increasing preventive funding. | NHS England, DHSC and ICBs | ⊕
Very low |
| Any funding should consider health equity to improve the efficiency and efficacy of spending. | NHS England, DHSC and ICBs | ⊕ ⊕ ⊕
Moderate |
| Where relevant, return on Investment tools should be used by local health and care systems to identify areas of highest efficiency for spending . | NHS England, DHSC and ICBs | ⊕ ⊕ ⊕ ⊕
High |
*GRADE certainty communicates the strength of evidence for each recommendation.
Recommendations which are supported by large trials will be graded highest whereas those arising from small studies or transferable evidence will be graded lower. The grading should not be interpreted as priority for policy implementation – i.e. some recommendations may have a low GRADE rating but likely to make a substantial difference.
How this brief was produced
What is the Living Evidence Map on what works to achieve equitable lipid management in primary care?
Using AI-powered software called EPPI-Reviewer, the Health Equity Evidence Centre has developed a Living Evidence Map of what works to address health inequalities in primary care. The software identifies research articles that examine interventions to address inequalities. The evidence map contains systematic reviews, umbrella reviews. More information can be found on the Health Equity Evidence Centre website.
Funding
This Evidence Brief has been commissioned by NHS England to support their statutory responsibilities to deliver equitable health care. Policy interventions beyond health care services were not in scope. The content of this brief was produced independently by the authors and do not necessarily reflect the views of NHS England.
Suggested citation
Holdroyd I, Dehn Lunn A, Diamond P, Harasgama S, Ghanchi A, Painter H, Pearce H, Torabi P, Vodden A, Wong YL, Ford J. Evidence brief: What works: Payment mechanisms to improve prevention spending in health care settings. Health Equity Evidence Centre; 2024
References
- Brown TT. How effective are public health departments at preventing mortality? Economics & Human Biology. 2014;13:34-45.
- Martin S, Lomas J, Claxton K. Is an ounce of prevention worth a pound of cure? A cross-sectional study of the impact of English public health grant on mortality and morbidity. BMJ Open. 2020;10(10):e036411.
- Owen L, Morgan A, Fischer A, Ellis S, Hoy A, Kelly MP. The costeffectiveness of public health interventions. Journal of Public Health. 2011;34(1):37-45.
- Singh SR. Public Health Spending and Population Health: A Systematic Review. American Journal of Preventive Medicine. 2014;47(5):634-40.
- Ford J, Ekeke N, Lahiri A, Kelly M. Making the case for prevention. 2021.
- Zwaagstra Salvado E, van Elten HJ, van Raaij EM. The Linkages Between Reimbursement and Prevention: A Mixed-Methods Approach. Front Public Health. 2021;9:750122.
- Jia L, Meng Q, Scott A, Yuan B, Zhang L. Payment methods for healthcare providers working in outpatient healthcare settings. Cochrane Database Syst Rev. 2021;1(1):CD011865.
- Stokes J, Bower P, Guthrie B, Mercer SW, Rice N, Ryan AM, et al. Cuts to local government spending, multimorbidity and healthrelated quality of life: A longitudinal ecological study in England. Lancet Reg Health Eur. 2022;19:100436.
- Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med. 1980;303(3):130-5.
- Patel. N GA, Vriend. M, Finch. D, Briggs. A. Options for restoring the public health grant: The Health Foundation; 2024
- Tao W, Agerholm J, Burström B. The impact of reimbursement systems on equity in access and quality of primary care: A systematic literature review. BMC Health Serv Res. 2016;16(1):542.
- Wranik D, Durier-Copp M. Framework for the design of physician remuneration methods in primary health care. Soc Work Public Health. 2011;26(3):231-59.
- Kiran T, Kopp A, Moineddin R, Glazier RH. Longitudinal evaluation of physician payment reform and team-based care for chronic disease management and prevention. Cmaj. 2015;187(17):E494-e502.
- Liddy C, Singh J, Hogg W, Dahrouge S, Taljaard M. Comparison of primary care models in the prevention of cardiovascular disease – a cross sectional study. BMC Fam Pract. 2011;12:114.
- Pearson WS, King DE, Richards C. Capitated payments to primary care providers and the delivery of patient education. J Am Board Fam Med. 2013;26(4):350-5.
- Matthews S, Qureshi N, Levin JS, Eberhart NK, Breslau J, McBain RK. Financial Interventions to Improve Screening in Primary Care: A Systematic Review. Am J Prev Med. 2024;67(1):134-46.
- Mauro M, Rotundo G, Giancotti M. Effect of financial incentives on breast, cervical and colorectal cancer screening delivery rates: Results from a systematic literature review. Health Policy. 2019;123(12):1210-20.
- Urwin S, Gillibrand S, Davies JC, Crosbie EJ. Factors associated with cervical screening coverage: a longitudinal analysis of English general practices from 2013 to 2022. Journal of Public Health. 2023;46(1):e43-e50.
- Van Herck P, De Smedt D, Annemans L, Remmen R, Rosenthal MB, Sermeus W. Systematic review: Effects, design choices, and context of pay-for-performance in health care. BMC health services research. 2010;10:247.
- Alshamsan R, Millett C, Majeed A, Khunti K. Has pay for performance improved the management of diabetes in the United Kingdom? Primary care diabetes. 2010;4(2):73-8.
- Mandavia R, Mehta N, Schilder A, Mossialos E. Effectiveness of UK provider financial incentives on quality of care: a systematic review. Br J Gen Pract. 2017;67(664):e800-e15.
- Steel N, Willems S. Research learning from the UK Quality and Outcomes Framework: a review of existing research. Quality in primary care. 2010;18(2):117-25.
- Mendelson A, Kondo K, Damberg C, Low A, Motúapuaka M, Freeman M, et al. The Effects of Pay-for-Performance Programs on Health, Health Care Use, and Processes of Care: A Systematic Review. Ann Intern Med. 2017;166(5):341-53.
- Ryan AM, Krinsky S, Kontopantelis E, Doran T. Long-term evidence for the effect of pay-for-performance in primary care on mortality in the UK: a population study. The Lancet. 2016;388(10041):268-74.
- Kontopantelis E, Springate DA, Ashworth M, Webb RT, Buchan IE, Doran T. Investigating the relationship between quality of primary care and premature mortality in England: a spatial wholepopulation study. Bmj. 2015;350:h904.
- Town R, Kane R, Johnson P, Butler M. Economic incentives and physicians’ delivery of preventive care: a systematic review. Am J Prev Med. 2005;28(2):234-40.
- Gillam SJ, Siriwardena AN, Steel N. Pay-for-performance in the United Kingdom: impact of the quality and outcomes framework: a systematic review. Annals of family medicine. 2012;10(5):461-8.
- Morales DR, Minchin M, Kontopantelis E, Roland M, Sutton M, Guthrie B. Estimated impact from the withdrawal of primary care financial incentives on selected indicators of quality of care in Scotland: controlled interrupted time series analysis. BMJ. 2023;380:e072098.
- Checkland K. Quality improvement in primary care. BMJ. 2023;380:p582.
- Mathes T, Pieper D, Morche J, Polus S, Jaschinski T, Eikermann M. Pay for performance for hospitals. Cochrane Database Syst Rev. 2019;7(7):Cd011156.
- Kim KM, Max W, White JS, Chapman SA, Muench U. Do penaltybased pay-for-performance programs improve surgical care more effectively than other payment strategies? A systematic review. Ann Med Surg (Lond). 2020;60:623-30.
- Fitzgerald JL. Social impact bonds and their application to preventive health. Aust Health Rev. 2013;37(2):199-204.
- Edmiston D, Nicholls A. Social Impact Bonds: The Role of Private Capital in Outcome-Based Commissioning. Journal of Social Policy. 2017;47(1):57-76.
- Hulse ESG, Atun R, McPake B, Lee JT. Use of social impact bonds in financing health systems responses to non-communicable diseases: scoping review. BMJ Global Health. 2021;6(3):e004127.
- Lowe T, Wilson R. Playing the Game of Outcomes-based Performance Management. Is Gamesmanship Inevitable? Evidence from Theory and Practice. Social Policy & Administration. 2017;51(7):981-1001.
- Tse AE, Warner ME. The razor’s edge: Social impact bonds and the financialization of early childhood services. Journal of Urban Affairs. 2018;42(6):816-32.
- Public Health England. Sexual and reproductive health: return on investment tool 2020
Available from: https://www.gov.uk/government/publications/sexual-and-reproductive-health-return-on-investment-tool - Public Health England. Return on investment tool: colorectal cancer 2016
Available from: https://www.gov.uk/government/publications/return-on-investment-tool-colorectal-cancer - Public Health England. Musculoskeletal conditions: return on investment tool 2017
Available from: https://www.gov.uk/government/publications/musculoskeletal-conditions-return-on-investment-tool - Office for Health Improvement and Disparities. Spend and outcomes tool (SPOT) 2020
Available from: https://www.gov.uk/government/publications/spend-and-outcome-tool-spot - Hewitt P. The Hewitt Review: An independent review into integrated care systems 2023
Available from: https://assets.publishing.service.gov.uk/media/642b07d87de82b00123134fa/the-hewitt-review.pdf - Demos. Revenue, Capital, Prevention 2023
Available from: https://demos.co.uk/wp-content/uploads/2023/09/PDEL-Briefing-paper_final-version.pdf - IPPR. HEALTHY PEOPLE, PROSPEROUS LIVES 2023
Available from: https://ippr-org.files.svdcdn.com/production/Downloads/1682577258_healthy-people-prosperous-lives-april-2023.pdf - Faculty of Public Health. A Prevention Transformation Fund. 2018.
- O’Mahony JF, Paulden M, McCabe C. NICE’s Discounting Review: Clear Thinking on Rational Revision Meets Obstacle of Industrial Interests. Pharmacoeconomics. 2021;39(2):139-46.
- Barr B, Bambra C, Whitehead M. The impact of NHS resource allocation policy on health inequalities in England 2001-11: longitudinal ecological study. BMJ. 2014;348:g3231.
- Holdroyd I, Appel C, Massou E, Ford J. Adjusting primary-care funding by deprivation: a cross-sectional study of lower-superoutput- areas in England. BJGP Open. 2024.