What works to improve health and digital literacy in disadvantaged groups

Digital health literacy is becoming increasingly important as more health information is shared through digital platforms. However, many individuals face challenges in accessing digital devices and understanding or critically evaluating digital health information. This evidence brief examines effective strategies for improving health and digital health literacy, particularly among disadvantaged groups.
What works to improve health and digital literacy in disadvantaged groups[PDF 353kb]
Download documentSummary
People living in the areas of greatest socioeconomic disadvantage and those from Black and Asian communities have the lowest levels of health literacy. Digital health literacy is becoming increasingly important with an increasing volume of health information being communicated via digital platforms and large numbers of people not just having poor access to digital devices but also struggling to understand and critically assess digital health information. Here we review the evidence for what works to improve health and digital health literacy in disadvantaged groups.
We reviewed 21 major studies examining health literacy and digital health literacy interventions. The evidence can be broadly divided into interventions targeted at five different groups: 1) people with low health literacy, 2) health literacy training for health professionals, 3) older people with low digital literacy, 4) ethnic minority groups and 5) people with mental health problems. There is strong evidence that health literacy interventions improve direct outcomes such as knowledge and understanding of health and care, especially using standard health literacy measures. While the long-term clinical outcomes are mixed, there are several large-scale studies which show positive outcomes. A range of digital and non-digital interventions are reflected in the literature and where available we present the evidence for what works in improving health and digital health literacy. Generally, the most effective interventions tailor information to the cultural and social needs of patients, engage with communities in the real-world setting, use a variety of multi-media tools, focus on upskilling and empowerment of patients and are delivered over a sustained period of time.
Current challenges
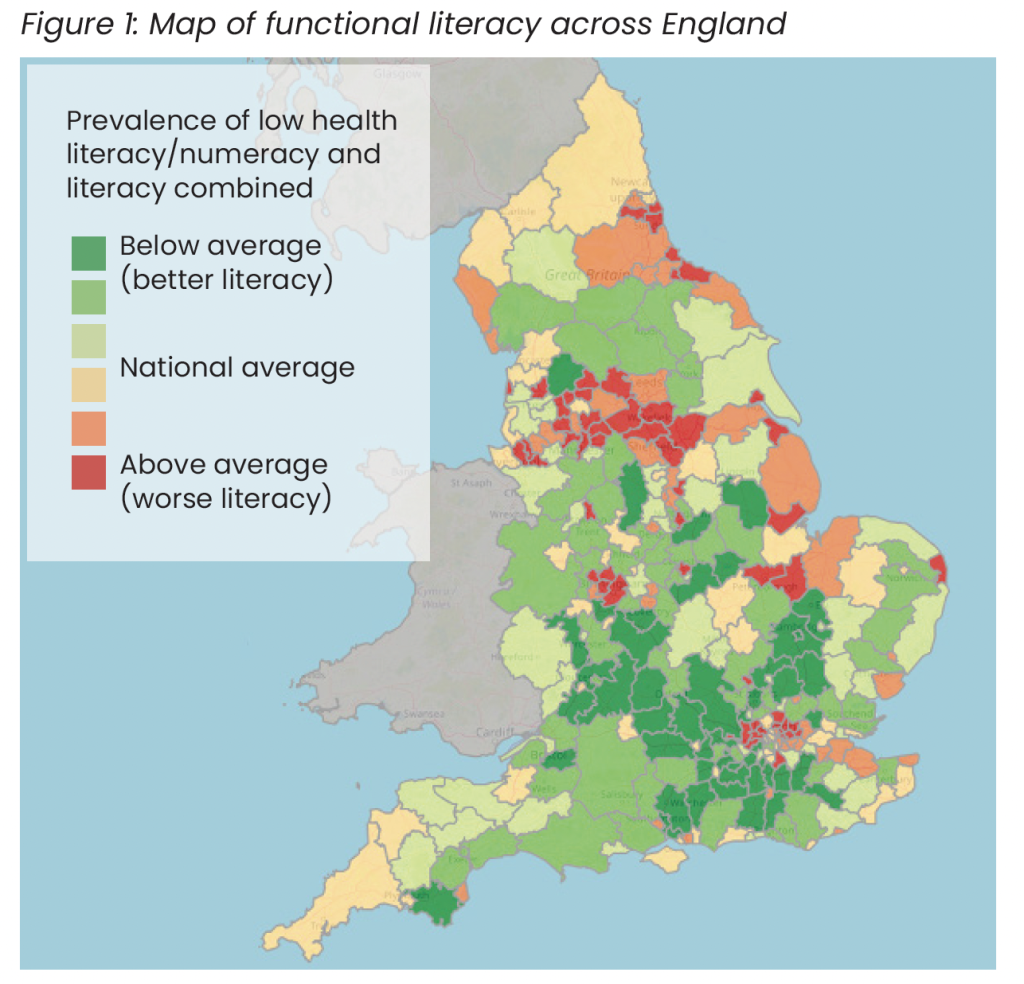
In the UK an estimated 43% of working age people do not understand health information involving text, rising to 61% when numeracy skills were included [1]. Poor health literacy, the ability to access and use health information (see Concepts box), is multifactorial but is often compounded by poor functional literacy i.e. reading, writing and numeracy skills. Low functional literacy is concentrated in urban areas of the north and northwest, northeast, West Midlands, certain London boroughs and more isolated areas including socioeconomically disadvantaged coastal communities [2].
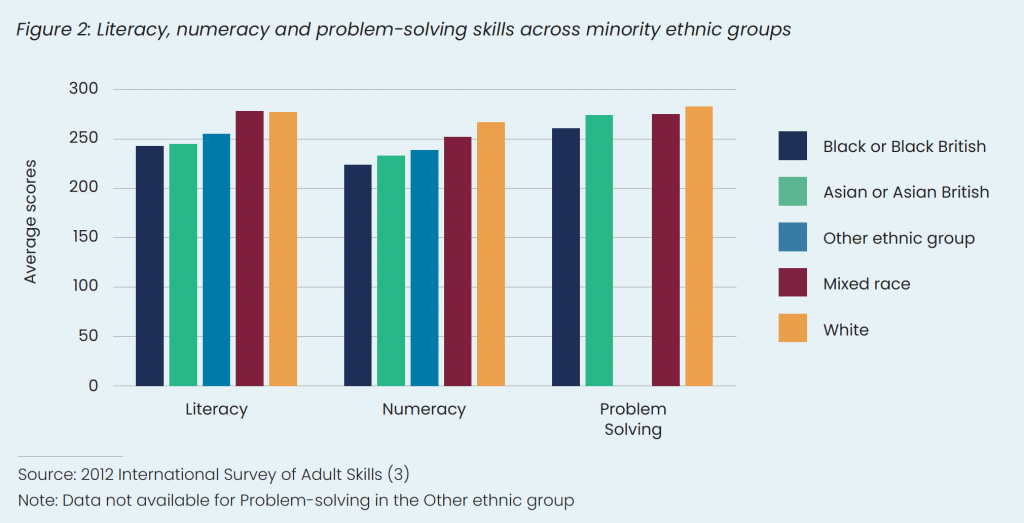
We do not have good data on health literacy across ethnic minority groups, however data does exist on functional literacy, numeracy and problem-solving skills in adults. The most accurate data were collected more than 10 years ago (2012 International Survey of Adult Skills) and showed adults from Black or Black British, Asian or Asian British and Other ethnic groups had lower literacy, numeracy and problem-solving skills compared to White and mixed race groups [3] – see Figure 2. People with multiple disadvantage, such as those belonging to ethnic minority groups, lower socioeconomic groups, older people, those with poor social networks and lower language proficiency are partly at risk of poor health and care outcomes related to lower health literacy [4][5].
Concepts
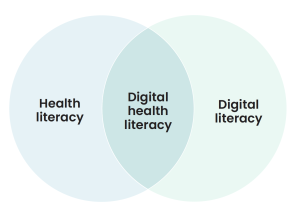
Different terms are used in the literature for different types of health and digital literacy. Here, we define health literacy as the ability of individuals to gain access to, understand and use information in ways which promote and maintain good health for themselves, their families and their communities [6].
Digital literacy is a broader concept than health. We define it as the ability to use information and communication technologies to find, evaluate, create, and communicate information, requiring both cognitive and technical skills [7].
Digital health literacy is the overlap between digital literacy and health literacy and defined as the ability to navigate the internet using electronic devices to find relevant information, access, understand and appraise health information including on social media and the ability to use digital interventions, such as mobile apps [8].
For people who do not speak English, health literacy should be distinguished from language proficiency. People who do not speak English may have poor health literacy in the context of the English language, but high health literacy in their native language.
Digital health literacy is the overlap between digital literacy and health literacy and defined as the ability to navigate the internet using electronic devices to find relevant information, access, understand and appraise health information including on social media and the ability to use digital interventions, such as mobile apps [8].
For people who do not speak English, health literacy should be distinguished from language proficiency. People who do not speak English may have poor health literacy in the context of the English language, but high health literacy in their native language.
Increasingly, good health literacy requires the ability to use electronic devices and digital skills to navigate health information. The proportion of households without internet access has remained unchanged since 2021 with 6% of UK adults not having access to the internet at home [9]. Using the latest data (from 2020), it is estimated that 3.3 million adults in the UK have never used the internet, 2.1 million of whom are over 75 years old [10]. People with low incomes are more likely to only access the internet using a smartphone; Ofcom found that 21% of people across the UK only access the internet using a smartphone and this increases to 31% for those on low incomes [11]. Beyond access to electronic devices and the internet, an estimated 6.8 million people (13%) having poor digital skills, especially older people, women and those on lower incomes [12].
A recent scoping review found a lack of evidence regarding the extent to which digital health interventions in the UK account for health inequalities in their design or outcomes [13]. It may be that poor health and/or digital literacy and/or limited digital access among disadvantaged groups limit the effectiveness of some digital interventions. Improving health and digital literacy may have the potential to narrow health inequality gaps through improving the knowledge, skills and confidence of using health information and digital tools in disadvantaged groups. Here we review the evidence for interventions which improve health and digital health literacy in disadvantaged groups, such as those on low incomes and ethnic minority groups.
What types of interventions have been described in the literature to improve health and digital literacy?
A recent review mapped the interventions to improve health literacy in disadvantaged groups, including using digital technology [14]. Based on 50 international studies, health literacy interventions include group education, practical exercises and games, role play, presentations, books, written handouts, videos, websites, and mobile applications. About half of studies included cultural tailoring, and 24 involved community or disadvantaged group representatives in the study development or delivery. Most programmes were delivered face-to-face with healthcare professionals or community health workers and were community-based, such as in community centres, faith-based organisations, or colleges, though some were delivered in primary care or at home.
Most interventions focused on functional health literacy (e.g., basic reading, writing, and factual information) and interactive health literacy (e.g., communicating and interacting with the health system), rather than critical health literacy (e.g., appraising the quality of health information) or scientific health literacy (e.g., understanding fundamental scientific concepts).
Summary of evidence
We reviewed 84 studies identified through the HEEC Living Evidence Maps (n=23), a complementary MEDLINE search that generated 1,796 records (n=49), and snowball searching (n=12). To identify the most relevant and robust evidence, we prioritised studies that were the most recent and high-quality systematic reviews, particularly those most relevant to the UK context. This resulted in 21 key studies synthesised in this brief.
Overall, there is good evidence that health literacy interventions directly improve the knowledge and skills of users, when assessed using validated health literacy measurement tools. While more distal clinical outcomes (such as weight, HbA1c or systolic blood pressure markers) have mixed data, there are several studies which show positive impacts on long-term health outcomes.
Several different health literacy interventions are described in the literature ranging from tailoring existing programmes for people with low health literacy, to bespoke community-based interventions for ethnic minority groups, older people, or people with mental health problems.
It was not possible to compare health literacy interventions to each other or draw firm conclusions about specific HL components because of the heterogeneity of study and intervention design. However, the most success interventions tailor information to patients, use a variety of multi-media tools, focus on upskilling and empowering users and are delivered over a sustained period of time.
Broadly, the literature was divided into five categories:
- People with low health literacy
- Health literacy training for health professionals
- Ethnic minority groups
- Older people with poor digital literacy
- People with mental health problems
1. People with low health literacy
Most studies examined ways to increase health literacy for people with poor health literacy. Patients who benefited from these interventions are more likely to be from lower socioeconomic groups [15][16]. Some studies explored health literacy interventions across multiple groups and services, whereas others focused on the health care setting, community setting or digital interventions.
In terms of studies which provided an overview of the literature, Taggart and colleagues conducted a landmark review in 2012 of interventions to improve health literacy in primary care [17]. Group education was the most common intervention (n = 15), and nutrition (n = 34) and physical activity (n = 32) the most common risk factors targeted. Of the 52 studies included, they found that 73% of interventions improved health literacy, and 75% improved outcomes related to smoking, nutrition, alcohol consumption, physical activity, or weight. Interventions with less than 3 hours of contact (such as use of tailored written material) were more likely to report positive impacts compared to those with more than 8 hours of contract (such as group education) (43% versus 33%). Smoking cessation health literacy interventions were more likely to be effective in primary care settings, whereas diet and physical activity interventions were more likely to be successful in the community. The study also found that people who participated in a health literacy intervention were 2.45 times more likely to have higher health literacy and 1.91 times more likely to complete treatment pathways.
More recently, Shao and colleagues (2023) undertook a meta-analysis of 18 studies examining health literacy interventions for people with chronic disease [18]. Interventions included group education sessions, social media interventions, education through multimedia (e.g. videos), one-on-one education and mobile apps. The authors found improvements in health literacy, mental well-being and self-efficacy. They did not find statistically significant improvements in Hb1Ac, but they did find improvements in blood pressure control. Another review by Samsiana and colleagues (2021) also found that health literacy for blood pressure control, such as web-based interventions, face-to-face training, workshops, and counselling, improved blood pressure outcomes in six of the seven included studies [19].
Walters and colleagues (2020) examined a range of health literacy interventions for changing health behaviours, particularly in terms of improving modifiable risk factors [20]. Based on 22 included studies, the authors found consistent evidence for improvements in smoking prevention, increased physical activity, cancer screening, nutrition, and diet-related behaviours. However, the authors did not specially focus on disadvantaged groups and therefore it is unclear if disadvantaged groups would benefit in the same way because they typically find it harder to make lifestyle changes in the setting of adverse social circumstances.
Healthcare based health literacy interventions
In the healthcare setting, an umbrella review by Larrotta-Castillo and colleagues (2023) reviewed 16 studies on the use of brochures, visual aids, digital tools, multimedia resources (videos), group and personalised counselling sessions in hospitals [21]. They found that nurses were the most common health professional group to deliver health literacy interventions and that interventions using pictograms reduced medication errors by caregivers significantly. Presenting information in multiple formats (e.g. verbal, written, digital and videos), video-based educational interventions and face-to-face visits by health professionals led to greater knowledge retention. However, the authors struggled to find evidence that these health literacy interventions increased empowerment.
A 2022 review by O’Cathain and colleagues mapped evidence of health literacy interventions to optimise A&E and primary care use [22]. Based on 67 articles, the authors examined seven interventions: navigation tools directing people to the range of services available (n = 7); written education about managing minor health problems in booklet or website format (n = 17); person-delivered education (n = 5); written education with person-delivered education (n = 17); multicomponent of written education, person-delivered education and mass media campaign (n = 5); self-triage (n = 9); and other (n = 7). Of 30 articles reporting impact on emergency department attendances, 19 (63%) showed a reduction, and 16/27 (59%) articles measuring impact on general practice consultations showed a reduction.
There is evidence that tailoring existing interventions for people with low health literacy can improve patient outcomes. Schapira and colleagues (2017) reviewed nine studies examining the tailoring of health and care information for people with low health literacy, such as reducing the reading level of material, online health literacy training, and support from a community health worker [23]. Five studies showed improvements in knowledge, management of long-term conditions, such as HbA1c, and depression. However, 2 studies in the review that focused on medication adherence did not find a statistically significant relationship between health literacy and adherence. Visscher and colleagues (2018) reviewed 23 studies of health literacy interventions and included three that explored tailoring existing interventions through presenting information according to different health literacy levels [24]. The authors found that the use of narrated animations, illustrated text, and audio-visual information led to better knowledge. However, Schaffler and colleagues (2018) found that tailoring information to support self-management for people who have low health literacy or low incomes was generally not effective [25]. This may be because the barriers to self-management for people with low incomes extend beyond simply not being able to access and use health information and are more fundamentally related to the social determinants of health.
Community based health literacy interventions
Harris and colleagues (2015) reviewed 144 studies of peer support to improve health literacy, through existing social networks, self-help groups, support groups or professional input. The authors found that peer support can improve the perception of themselves as individuals with low literacy, which in turn empowers them to increase healthy behaviours and self-management attitudes [26]. This may be because socially vulnerable people can trust their peers more and build meaningful relationships with them. This ‘bottom-up’ approach of learning from peers rather than health experts can see more effective results in improving health literacy. More relevant information can be found in our complementary community engagement and empowerment evidence brief.
A review examined the role of librarians, both in community and clinical settings, in supporting health literacy. Vassilakaki and colleagues (2022) reviewed 31 research studies examining how librarians support health literacy and found examples of librarians helping members of the public through group-based interventions, assisting clinical teams in understanding the literature on health literacy, supporting the co-design of health literacy interventions, and aiding research [27]. However, isolating the contribution of librarians in the context of a multicomponent intervention was difficult.
Digital health literacy
There has been a proliferation of digital interventions, but few consider digital health literacy. Cheng and colleagues (2020) examined 51 studies evaluating digital health interventions for older people, ethnic minority groups, low-income, low-literacy, and rural communities [28].
None of the included studies considered digital health literacy in their development, user involvement was minimal, and few included strategies to help users engage with the interventions. In those studies that did include a digital health literacy component, the focus tended to be on the use of health information and understanding health concepts, rather than tailoring digital interventions to individual needs or ensuring that people could engage with the interventions.
Verweel and colleagues (2023) reviewed 16 randomised controlled trials with over 5,000 people with chronic conditions [29]. The authors explored the interventions through a digital health literacy lens, and examined online self-management training, electronic health record training and remote patient monitoring. The authors found that interventions augmented with patients’ electronic patient records were most effective at improving digital health literacy. Finally, Refahi and colleagues (2023), based on five studies including online group training with in-person support, found a positive impact of educational interventions on self-reported digital health literacy skills [30].
2. Health literacy training for health professionals
Several studies focused on health literacy training of health professionals. Saunders and colleagues (2017) reviewed 28 studies on training delivered to health professional students in universities and colleges [31]. Interventions ranged from large group lectures to community placements and aimed to help health professionals communicate better with patients with low health literacy. The included studies were generally of poor design. The most successful interventions offered numerous training sessions and integrated knowledge and skill acquisition, particularly when developed within real-world settings with patients or community members.
Ayre and colleagues (2023) reviewed the evidence on training health literacy champions [32]. They reviewed five studies on increasing organisational awareness and commitment, or influencing strategic and operational planning. Two of the four studies found positive impacts, such as more patients and family receiving information about their health condition.
3. Ethnic minority groups
Health literacy
We found only limited evidence focusing on ethnic minority groups and health literacy. Singh and colleagues (2024) reviewed 55 studies exploring health literacy interventions, with key findings for ethnic minority groups [33]. They found that the most effective interventions assessed needs of participants through focus groups prior to conducting the intervention, used bilingual educational materials, and included professionals fluent in the first languages of patients. The authors argued that it is important to distinguish literacy needs from language proficiency because some people may have high literacy skills but might not be language proficient.
Of the 48 studies that Romanova and colleagues (2024) included in a review on examining health literacy interventions for disadvantaged groups, 11 focused on ethnic or racial minorities [14]. Interventions ranged from culturally relevant written material with or without videos, face-to-face teaching sessions, online storytelling, games, and church-based sermons raising awareness of HIV. Two of the interventions were co-designed with members of the community. All studies reported improvements in health literacy, as measured by knowledge or health literacy metrics, but only one study reported clinical outcomes and found no difference between intervention and control.
A systematic review of health literacy interventions among Spanish-speaking populations in the US may have transferable evidence for the UK context. Hernandez and colleagues (2024) examined 62 studies across both community and clinical settings [34]. About half of the interventions included in-person education and used multimedia education. Most studies (89%) reported improvements in health literacy, as well as improvements in some clinical outcomes such as weight, HbA1c, and blood pressure. The researchers found that the most successful strategies included professional liaison support, such as community health workers, and multimedia material, such as linguistically and culturally adapted photo comics.
Digital Health literacy
Two reviews published in 2023 examined the role of digital health literacy interventions for South Asian communities. Aldosari and colleagues undertook a scoping review and included 15 articles [4]. The authors found consistent evidence that South Asian communities, especially older people in these communities, struggle to use digital interventions. They identified that low proficiency in English was a barrier, and even when resources were translated, they were often in a formal style that was difficult to understand. Other barriers identified included a lack of trust in digital technology, gender roles (with men more likely to use technology than women), and time constraints. Few studies were found that quantitatively examined the impact of digital health literacy interventions, but the authors were able to identify principles more likely associated with success based on mixed-method evidence. These included the development of multilingual and culturally sensitive interventions in trusted community locations, such as faith organisations, and digital skill development sessions.
Goswami and colleagues undertook a realist review of digital health interventions to prevent cardiovascular disease and diabetes in South Asian communities [5]. Similarly, the authors found barriers including personal beliefs, social networks, education, and material circumstances. They found that the user interface and experience, with visual instructions rather than text, culturally tailored interventions, and integration into existing health and care services were key.
4. Older people with poor digital literacy
Transferable insights for disadvantaged groups may be found through exploring the literature for digital health literacy interventions in older people. Zolbin and colleagues (2022) published a systematic review including 34 studies focused on digital health literacy in older people [35]. Most interventions were delivered in person within the community (n=22) compared to online (n=12). The authors found that successful interventions required access to technology, IT skills development, and a focus on empowering older people to use the technology rather than allowing someone else to do it for them. A review published in 2014 by Watkins and colleagues found that collaborative and tailored approaches were most effective in improving digital health literacy in older people [36]. They found broad support for interventions improving digital health literacy through validated measures but noted the lack of high-quality studies.
Dong and colleagues (2023) undertook a meta-analysis with seven studies exploring digital health literacy interventions over 2-8 weeks in older people; three studies examined an in-person intervention and four were online [37]. The meta-analysis of predominantly US studies found that digital health literacy interventions had a positive overall effect on health literacy, but those that were in person, guided by a conceptual framework, and sustained over more than four weeks had a greater likelihood of success.
5. People with mental health problems
Digital mental health literacy interventions aim to enhance knowledge and beliefs about mental disorders, thereby assisting in their recognition, management, or prevention through digital means. These interventions have been hailed as way of helping to address the mismatch between demand and capacity in mental health services. The technology has evolved from conventional platforms, such as films, videos, multimedia, and emails, to more modern, interactive platforms, including mobile apps, web-based or internet platforms, and social media.
Yeo and colleagues (2024) collated evidence about digital mental health literacy interventions in a review and meta-analysis of 144 articles [38]. In their meta-analysis, the authors found that such interventions, when examined in a before-and-after design, had a large, statistically significant effect on digital health literacy measures and a small but statistically significant effect on mental health outcomes. The authors also found that digital mental health literacy interventions were as effective as traditional face-to-face mental health literacy interventions. Moreover, digital mental health literacy interventions that were augmented with another intervention (such as face-to-face CBT) proved more effective than those delivered alone. The platform and frequency of use did not appear to affect the results.
Limitations
The pace of technological advancement is outstripping researchers’ ability to explore and evaluate digital interventions. Equally the plethora of different interventions, platforms and services available makes it impossible to accurately compare one intervention compared to another. The interventions studies are also highly dependent on the health care setting and population groups. For example, health literacy interventions for south Asian populations to improve cardiovascular disease will be different to interventions to improve mental health literacy for lower socioeconomic groups. However, there are clear principles in the data which are associated with success and these are presented in this evidence brief.
What works: Key recommendations
| Recommendation | Target audience | GRADE certainty |
|
Existing programmes, services and communication should be tailored so that the content is easy to understand for people with low health literacy. e.g., by working with patient representatives to ensure written material is understandable. |
NHS England, ICBs, PCNs, Trusts, pharmacies and GPs |
⊕ ⊕ ⊕
Moderate |
|
Patient education material should use pictograms, illustrated text, and narrated animations and audio-visual information (in digital material) as much as possible, rather than only relying on text. |
NHS England, ICBs, PCNs, Trusts, pharmacies and GPs |
⊕ ⊕ ⊕
Moderate |
|
Health professional training on health literacy should be delivered over several sessions and co-developed with community members within real-world settings. |
NHS England, ICBs, PCNs, Trusts, pharmacies and GPs |
⊕ ⊕ ⊕
Moderate |
|
Services and programmes which seek to improve health literacy should provide users with information in multiple languages and delivered by staff from local communities or community health workers. |
NHS England, ICBs, PCNs, Trusts, pharmacies and GPs |
⊕ ⊕ ⊕
Moderate |
|
Digital health literacy programmes should be delivered in familiar community settings, tailored to users’ cultural and social needs and integrated into local health and care services. |
NHS England, ICBs, PCNs, Trusts, pharmacies and GPs |
⊕ ⊕ ⊕
Moderate |
|
Programmes for older people should focus on improving access, upskilling and empowering users over a sustained period. |
NHS England, ICBs, PCNs, Trusts, pharmacies and GPs |
⊕ ⊕ ⊕
Moderate |
|
Consider health literacy champions to raise awareness and influence strategic and operational planning within organisations. |
NHS England, ICBs, PCNs, Trusts, pharmacies and GPs |
⊕ ⊕
Low |
|
If relevant, undertake digital health literacy interventions alongside access to an individual’s electronic health records to help users understand the use of the tool in the context of their own health record. |
NHS England, ICBs, PCNs, Trusts, pharmacies and GPs |
⊕ ⊕
Low |
|
Digital mental health literacy interventions are as effective as face-to-face health literacy interventions, especially when augmented with other services, and should be used to improve access where demand exceeds capacity. |
NHS England, ICBs, Trusts |
⊕ ⊕
Low |
|
Where possible, library services should be leveraged in the community to improve health literacy. |
NHS England, ICBs |
⊕
Very low |
*GRADE certainty communicates the strength of evidence for each recommendation [39]. Recommendations which are supported by large trials will be graded highest whereas those arising from small studies or transferable evidence will be graded lower. The grading should not be interpreted as priority for policy implementation – i.e. some recommendations may have a low GRADE rating but likely to make a substantial population impact.
Useful links
How this brief was produced
What is the Living Evidence Map on what works to achieve equitable lipid management in primary care?
Using AI-powered software called EPPI-Reviewer, the Health Equity Evidence Centre has developed a Living Evidence Map of what works to address health inequalities in primary care. The software identifies research articles that examine interventions to address inequalities. The evidence map contains systematic reviews, umbrella reviews. More information can be found on the Health Equity Evidence Centre website.
Funding
This Evidence Brief has been commissioned by NHS England to support their statutory responsibilities to deliver equitable health care. Policy interventions beyond health care services were not in scope. DL is funded by NIHR ARC North Thames. The views expressed in this publication are those of the author(s) and not necessarily those of NHS England or NIHR.
Suggested citation
Harasgama S, Dehn Lunn A, Lamb D, Gkiouleka A, Painter H, Ford J. Evidence brief: What works to improve health and digital literacy in disadvantaged groups. Health Equity Evidence Centre; 2024
References
- Rowlands G, Protheroe J, Winkley J, Richardson M, Seed PT, Rudd R. A mismatch between population health literacy and the complexity of health information: an observational study. Br J Gen Pract. 2015 Jun;65(635):e379-386.
- University of Southampton. Health Literacy: Prevalence Estimates for Local Authorities [Internet]. 2024 [cited 2024 Aug 30].
Available from: https://healthliteracy.geodata.uk/ - Department for Business, Innovation & Skills. GOV.UK. [cited 2024 Aug 30]. Adult skills international survey 2012.
Available from: https://www.gov.uk/government/publications/international-%20survey-of-adult-skills-2012 - Aldosari Nasser, Ahmed Saima, McDermott Jane, Stanmore Emma. The Use of Digital Health by South Asian Communities: Scoping Review. Journal of medical Internet research. 2023;25:e40425.
- Goswami Aumeya, Poole Lydia, Thorlu-Bangura Zareen, Khan Nushrat, Hanif Wasim, Khunti Kamlesh, et al. The Use of Digital Health Interventions for Cardiometabolic Diseases Among South Asian and Black Minority Ethnic Groups: Realist Review. Journal Of Medical Internet Research. 2023;25:e40630–e40630.
- World Health Organisation. Health literacy [Internet]. 2024 [cited 2024 Aug 30].
Available from: https://www.who.int/teams/%20health-promotion/enhanced-wellbeing/ninth-global-conference/%20health-literacy - UNESCO Institute for Information Technologies in Education. Digital Literacy in Education [Internet]. 2011 [cited 2024 Aug 30].
Available from: https://iite.unesco.org/pics/publications/en/%20files/3214688.pdf - Norman CD, Skinner HA. eHealth Literacy: Essential Skills for Consumer Health in a Networked World. J Med Internet Res. 2006 Jun 16;8(2):e9.
- Ofcom. Adults’ media use and attitudes 2024: interactive report [Internet]. 2024 [cited 2024 Aug 30].
Available from: https://%20www.ofcom.org.uk/media-use-and-attitudes/media-habits-%20adults/adults-media-use-and-attitudes-2024-interactive-%20report/ - Office for National Statistics. Internet users, UK [Internet]. 2021 [cited 2024 Aug 30].
Available from: https://www.ons.gov.uk/%20businessindustryandtrade/itandinternetindustry/bulletins/internetusers/%202020 - Ofcom. Adults’ media use and attitudes 2022 [Internet]. 2022 [cited 2024 Aug 30].
Available from: https://www.ofcom.org.%20uk/media-use-and-attitudes/media-habits-adults/interactive-%20tool/ - Lloyds Bank. 2023 Consumer Digital Index: The UK’s largest study of digital and financial lives [Internet]. 2023 [cited 2024 Aug 30].
Available from: https://www.lloydsbank.com/%20assets/media/pdfs/banking_with_us/whats-happening/%20231122-lloyds-consumer-digital-index-2023-report.pdf - Farre A, Fang M, Hannah B, Makita M, McFadden A, Menezes D, et al. Exploring the use of digital technology to deliver healthcare services with explicit consideration of health inequalities in UK settings: A scoping review. Digit Health. 2023 Jun 29;9:20552076231185442.
- Romanova A, Rubinelli S, Diviani N. Improving health and scientific literacy in disadvantaged groups: A scoping review of interventions. Patient Educ Couns. 2024 May;122:108168.
- Gibney S, Bruton L, Ryan C, Doyle G, Rowlands G. Increasing Health Literacy May Reduce Health Inequalities: Evidence from a National Population Survey in Ireland. Int J Environ Res Public Health. 2020 Aug;17(16):5891.
- Svendsen MT, Bak CK, Sørensen K, Pelikan J, Riddersholm SJ, Skals RK, et al. Associations of health literacy with socioeconomic position, health risk behavior, and health status: a large national population-based survey among Danish adults. BMC Public Health. 2020 Apr 28;20(1):565.
- Taggart Jane, Williams Anna, Dennis Sarah, Newall Anthony T, Shortus Tim, Zwar Nicholas, et al. A systematic review of interventions in primary care to improve health literacy for chronic disease behavioral risk factors. BMC Family Practice [Internet]. 2012;13(1).
Available from: https://explore.openalex.org/works/%20W2114750812 - Shao Y, Hu H, Liang Y, Hong Y, Yu Y, Liu C, et al. Health literacy interventions among patients with chronic diseases: A meta- analysis of randomized controlled trials. Patient Educ Couns. 2023 Sep;114:107829.
- Samsiana S, Russeng SS, Amiruddin R. Intervention Based on Integration of Health Literacy and Health Outcomes in Hypertension “A Systematic Review”. Open Access Macedonian Journal of Medical Sciences. 2021 Jan 10;9(F):486–91.
- Walters R, Leslie SJ, Polson R, Cusack T, Gorely T. Establishing the efficacy of interventions to improve health literacy and health behaviours: a systematic review. BMC Public Health. 2020 Jun 30;20(1):1040.
- Larrotta-Castillo D, Moreno-Chaparro J, Amaya-Moreno A, Gaitán-Duarte H, Estrada-Orozco K. Health literacy interventions in the hospital setting: an overview. Health Promot Int. 2023 Jun 1;38(3):daac043.
- O’Cathain A, Foster A, Carroll C, Preston L, Ogden M, Clowes M, et al. Health literacy interventions for reducing the use of primary and emergency services for minor health problems: a systematic review [Internet]. Southampton (UK): National Institute for Health and Care Research; 2022 [cited 2024 Aug 30]. (Health and Social Care Delivery Research).
Available from: http://www.%20ncbi.nlm.nih.gov/books/NBK587674/ - Schapira Marilyn M, Swartz Sheila, Ganschow Pamela, Jacobs Elizabeth A, Neuner Joan, Walker Cindy M, et al. Tailoring Educational and Behavioral Interventions to Level of Health Literacy: A Systematic Review. MDM Policy & Practice. 2017;2(1):238146831771447–238146831771447.
- Visscher BB, Steunenberg B, Heijmans M, Hofstede JM, Devillé W, van der Heide I, et al. Evidence on the effectiveness of health literacy interventions in the EU: a systematic review. BMC Public Health. 2018 Dec 29;18(1):1414.
- Schaffler J, Leung K, Tremblay S, Merdsoy L, Belzile E, Lambrou A, et al. The Effectiveness of Self-Management Interventions for Individuals with Low Health Literacy and/or Low Income: A Descriptive Systematic Review. J Gen Intern Med. 2018 Apr;33(4):510–23.
- Harris J, Springett J, Croot L, Booth A, Campbell F, Thompson J, et al. Can community-based peer support promote health literacy and reduce inequalities? A realist review [Internet]. Southampton (UK): NIHR Journals Library; 2015 [cited 2024 Aug 23]. (Public Health Research).
Available from: http://www.ncbi.nlm.nih.gov/%20books/NBK274412/ - Vassilakaki E, Moniarou-Papaconstaninou V. Librarians’ support in improving health literacy: A systematic literature review. Journal of Librarianship and Information Science. 2023 Jun 1;55(2):500–14.
- Cheng C, Beauchamp A, Elsworth GR, Osborne RH. Applying the Electronic Health Literacy Lens: Systematic Review of Electronic Health Interventions Targeted at Socially Disadvantaged Groups. J Med Internet Res. 2020 Aug 13;22(8):e18476.
- Verweel L, Newman A, Michaelchuk W, Packham T, Goldstein R, Brooks D. The effect of digital interventions on related health literacy and skills for individuals living with chronic diseases: A systematic review and meta-analysis. International Journal of Medical Informatics. 2023 Sep 1;177:105114.
- Refahi H, Klein M, Feigerlova E. e-Health Literacy Skills in People with Chronic Diseases and What Do the Measurements Tell Us: A Scoping Review. Telemedicine and e-Health. 2023 Feb;29(2):198–208.
- Saunders C, Palesy D, Lewis J. Systematic Review and Conceptual Framework for Health Literacy Training in Health Professions Education. Health Professions Education. 2019 Mar 1;5(1):13–29.
- Ayre J, Zhang M, Mouwad D, Zachariah D, McCaffery KJ, Muscat DM. Systematic review of health literacy champions: who, what and how? Health Promotion International. 2023 Aug 1;38(4):daad074.
- Singh H, Samkange-Zeeb F, Kolschen J, Herrmann R, Hübner W, Barnils NP, et al. Interventions to promote health literacy among working-age populations experiencing socioeconomic disadvantage: systematic review. Front Public Health. 2024;12:1332720.
- Hernandez J, Demiranda L, Perisetla P, Andrews L, Zhang K, Henderson R, et al. A systematic review and narrative synthesis of health literacy interventions among Spanish speaking populations in the United States. BMC Public Health. 2024 Jun 27;24(1):1713.
- Ghorbanian Zolbin M, Huvila I, Nikou S. Health literacy, health literacy interventions and decision-making: a systematic literature review. Journal of Documentation. 2022 Jan 1;78(7):405–28.
- Watkins I, Xie B. eHealth Literacy Interventions for Older Adults: A Systematic Review of the Literature. Journal of Medical Internet Research. 2014 Nov 7;16(11):e3318.
- Dong Q, Liu T, Liu R, Yang H, Liu C. Effectiveness of Digital Health Literacy Interventions in Older Adults: Single-Arm Meta-Analysis. Journal of Medical Internet Research. 2023 Jun 28;25(1):e48166.
- Yeo G, Reich SM, Liaw NA, Chia EYM. The Effect of Digital Mental Health Literacy Interventions on Mental Health: Systematic Review and Meta-Analysis. J Med Internet Res. 2024 Feb 29;26:e51268.
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso- Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008 Apr 24;336(7650):924–6.