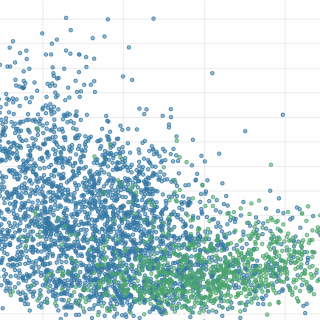
How does the age structure of patients affect NHS payments to General Practice?
In 2023/24, 6,669 practices received £10.2 billion from the NHS. Capitation payments to individual practices are adjusted using the Carr-Hill formula. On average, practices received £164.64 per patient, with higher payments for practices serving older populations due to higher healthcare needs, prescribing costs and the specific needs of rural areas. This analysis explores how NHS payments to general practices are informed by the age structure, deprivation and rurality of registered patients.